If counting respirations feels more challenging than it should, you’re experiencing what CNA students consistently report. This seemingly simple CNA skill requires precision that can make or break your testing success.
Understanding exactly what evaluators look for across all testing providers can transform your confidence from anxiety into competence.
Students often discover that respiratory assessment combines technical accuracy with subtle observation skills. The ±2 breath margin for error might seem generous, but achieving that consistency under testing pressure requires genuine preparation. Current 2025 protocols across NNAAP, Prometric, and Headmaster maintain strict standards that demand both procedural knowledge and practical technique mastery.
What CNAs Need to Know About Respiration Counting Requirements
One CNA community member shared: “Counting respirations is one of the hardest things.” This validation reflects the genuine complexity behind what appears straightforward. Testing providers require absolute accuracy within ±2 breaths of the evaluator’s count, making precision essential for passing.
The universal 60-second counting requirement prevents shortcuts that compromise accuracy. Students cannot count to 30 seconds or multiply by two. Evaluators watch for this full-minute commitment while simultaneously conducting their own count for comparison.
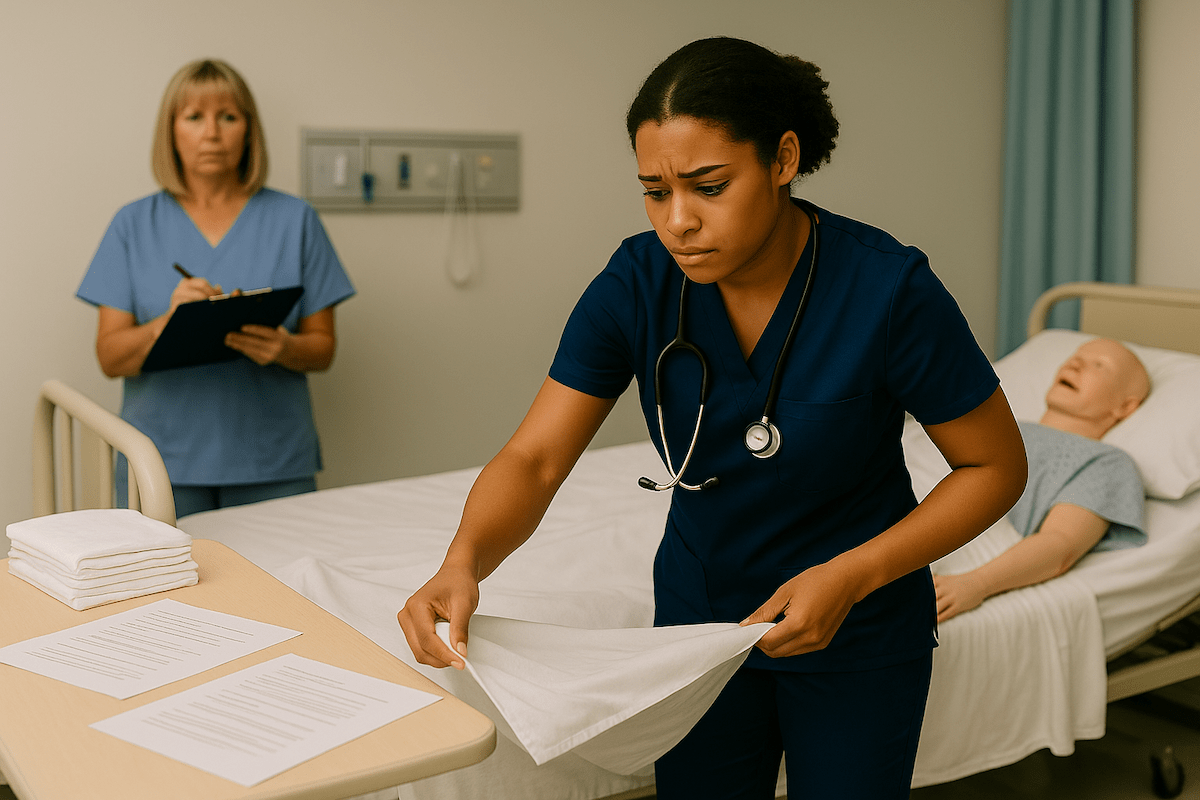
Discreet observation forms the cornerstone of accurate respiratory assessment. As students frequently mention: “Their breathing will change if they know you’re counting.” Research confirms that conscious awareness of breathing monitoring alters natural patterns, making stealth essential for authentic measurements.
All three major testing providers maintain identical accuracy standards regardless of their procedural variations. Whether testing through NNAAP, Prometric, or Headmaster, the±2 breath tolerance remains constant.
Master This Skill With Expert Video Guides
Join 6,000,000+ students who passed with Mometrix’s proven study system
Get Instant Access →Step-by-Step Respiration Counting Technique for CNA Testing
Mastering respiratory assessment requires systematic positioning and timing that maintains patient comfort while ensuring measurement accuracy. Follow these six essential steps for confident testing performance:
Master CNA respiration rate measurement with this 6-step discreet counting technique used by 11,000+ successful test candidates. Ensures accurate 60-second timing and prevents patient awareness that could alter natural breathing patterns.
- Position for Clear Chest Observation
Stand or sit where you can clearly observe chest movement without creating patient discomfort. The chest provides the most reliable visual indicator, though shoulder or abdominal movement can substitute when chest observation is limited.
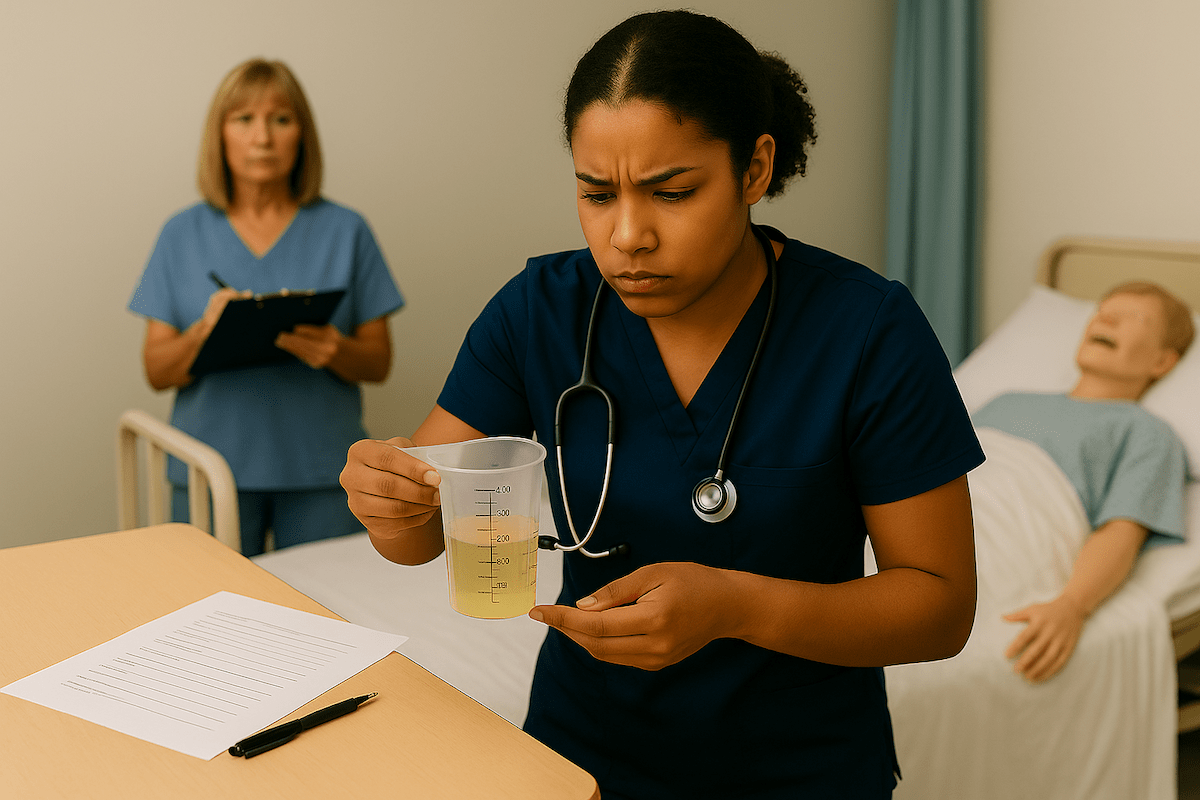
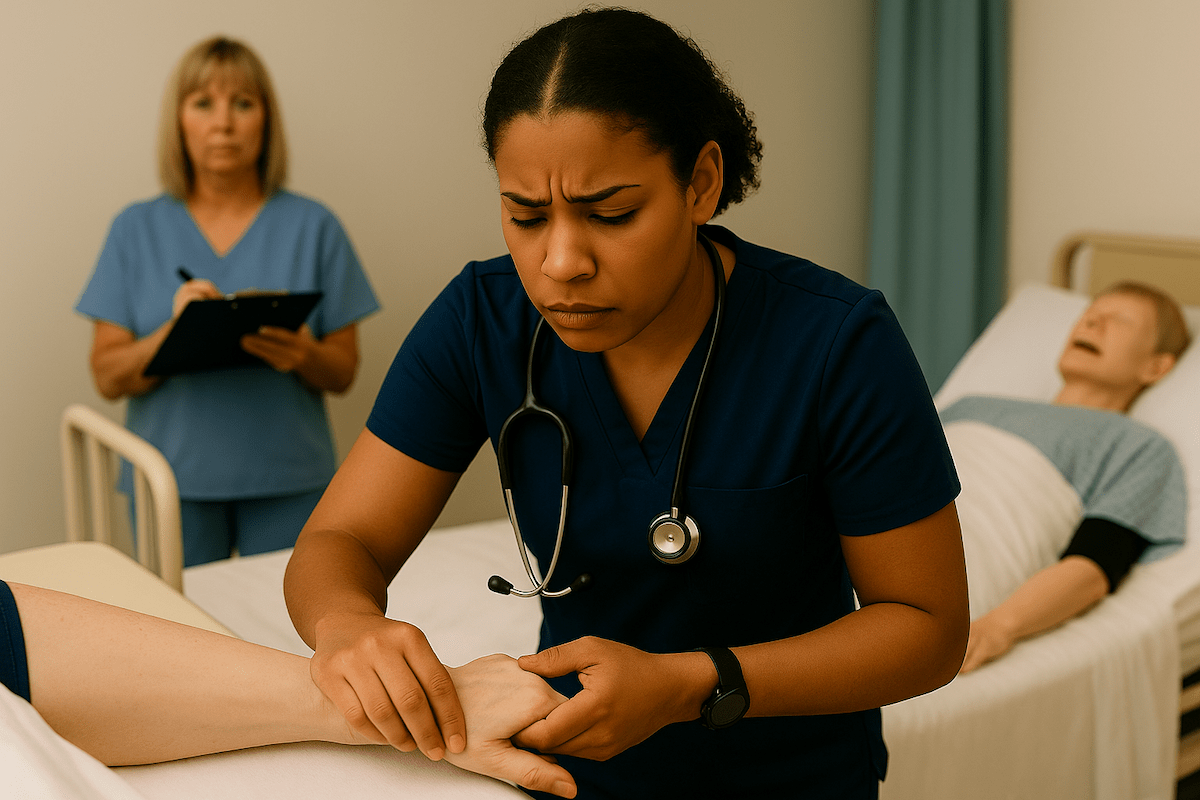
- Establish Discreet Hand Positioning
Hold the patient’s wrist as if taking their pulse. This positioning allows natural respiration observation without alerting the patient to your counting focus and prevents altered breathing patterns.
- Define One Complete Respiration Cycle
Count one full inhale-exhale cycle as one respiration. Watch for the complete chest rise and fall pattern rather than counting individual breaths separately to ensure accurate measurement.
- Maintain Accurate 60-Second Timing
Use your watch’s second hand or internal timing to ensure exactly 60 seconds duration. Testing providers verify timing precision, making this accuracy crucial for passing the evaluation.
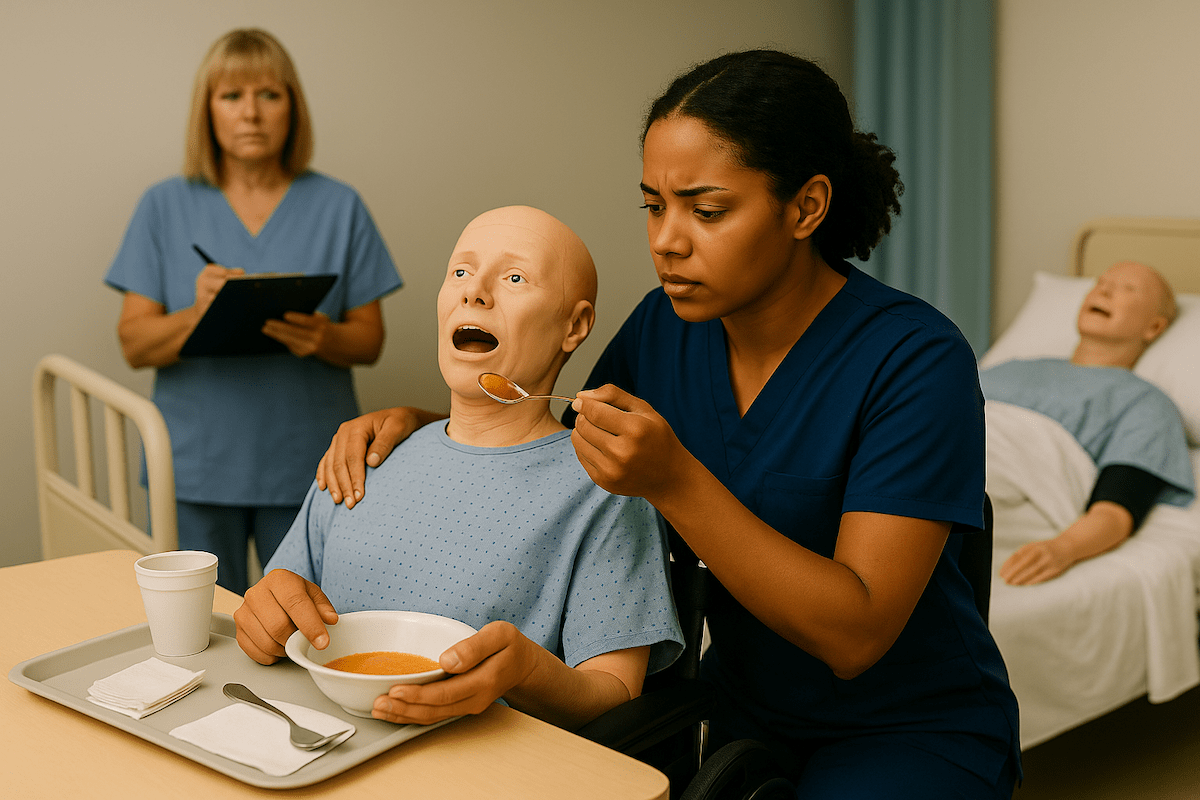
- Continue Natural Demeanor Throughout
Maintain casual conversation or comfortable silence throughout the counting period. Your demeanor should appear relaxed and routine to prevent patient awareness that could alter natural breathing.
- Record Measurement Immediately
Document your count immediately after completing the 60 seconds. Hand hygiene precedes recording, following standard infection control protocols required by all testing providers.
Handling Challenging Counting Situations During Skills Tests
Real testing environments present obstacles that classroom practice cannot fully simulate. Common challenges include:
- Moving or restless patients – Shift your observation angle without alerting evaluators to difficulties
- Lost count recovery – Continue observing while mentally estimating where you stopped
- Patient questions – Respond with “I’m checking your vital signs” rather than mentioning breathing
- Irregular breathing patterns – Count each complete cycle regardless of rhythm variations
Students consistently report: “Sometimes you genuinely can’t get a good respiration count, especially if they’re moving.” These situations require calm professionalism and adaptation strategies rather than obvious restart behaviors that signal problems to evaluators.
As CNAs frequently encounter: “Sometimes they will get annoyed and say, ‘Why are you standing there watching me like that?'” Professional responses that maintain assessment integrity while reassuring patients help complete accurate measurements without compromising the evaluation process.
Workflow Efficiency: Integrating Respiration Counting with Other Vital Signs
Sequential vital signs measurement maximizes testing time while maintaining accuracy standards. Key efficiency strategies include:
- Seamless transitions – Move from pulse to respiration counting while maintaining wrist contact
- Equipment coordination – Use BP cuff inflation time for respiration counting when appropriate
- Strategic timing – Plan hand hygiene between measurements without rushing for accuracy
- Documentation workflow – Record measurements immediately to prevent memory errors
As one community member noted: “Do the respiration count while the BP cuff is going.” This timing strategy optimizes evaluation periods while maintaining individual measurement integrity.
Many CNAs discover that pulse measurement naturally transitions to respiration counting. After completing the pulse assessment, maintain wrist contact while shifting attention to chest observation. This seamless transition prevents patient awareness while supporting accurate timing.
Provider-Specific Testing Requirements: NNAAP vs. Prometric vs. Headmaster
Understanding provider variations prevents confusion during actual testing while ensuring technique alignment with specific evaluation expectations. Current 2025 protocols reflect both standard practices and lingering pandemic adaptations.
Provider Comparison Table:
| Provider | Skill Format | Timing Communication | Key Requirement |
| NNAAP | Standalone skill | Silent timing | ±2 breath accuracy |
| Prometric | Separate from pulse | No verbal cues to the patient | Record on the provided form |
| Headmaster | Combined with pulse | “Start/stop” announcements | Sequential measurement |
NNAAP Requirements:
- Standalone skill separate from pulse measurement
- Silent timing approach without verbal announcements
- State-specific mask policies vary by location
- Standard ±2 breath accuracy evaluation
Prometric Standards:
- Explicit instruction not to cue patient breathing patterns
- Recording form documentation with specific format requirements
- COVID-era adaptations are active in select locations
- Separate respiration skill testing format
Headmaster Protocols:
- Combined pulse and respiration measurement scenarios
- Verbal “start” and “stop” announcements to evaluators are required
- Sequential measurement with smooth transitions
- Contingency COVID protocols available for high-exposure situations
Practice With 600+ CNA Exam Questions
See exactly how this skill appears on the real test
Respiration Counting Interactive CNA Skill Checklist
Practice makes perfect, and having a reference guide during your preparation sessions helps build the muscle memory you need for testing day. Use this interactive checklist during practice to ensure you’re hitting every critical step evaluators watch for.
Managing Test Anxiety and Observation Pressure During Respiration Assessment
Performance anxiety affects both measurement accuracy and the quality of patient interaction. Understanding these psychological factors helps students develop effective coping strategies:
- Observation pressure awareness – Both students and patients experience heightened stress during evaluation
- Evaluator training recognition – Testing staff receive instruction to observe professionally without adding pressure
- Practice under pressure – Simulated testing conditions build confidence more than general study
- Mental focus strategies – Internal timing methods and count-tracking techniques prevent distraction
Research confirms that observation pressure impacts both students and patients during assessment procedures. Students experience heightened awareness of evaluator scrutiny, while patients may unconsciously alter breathing when they sense focused attention.
Building confidence requires practice under simulated pressure conditions that mirror actual testing environments. Professional preparation includes developing mental strategies for maintaining focus during the full 60-second counting period.
Respiration Counting Video Demonstration
Seeing proper respiration counting technique helps many students understand the subtle positioning and timing elements that written instructions alone can’t fully capture. This demonstration shows you exactly what evaluators expect during testing.
Respiration Counting FAQ for CNA Students
Count respirations for exactly 60 seconds. All testing providers require full-minute timing without shortcuts. Counting for 30 seconds and multiplying by two is not acceptable.
Your recorded count must be within ±2 breaths of the evaluator’s measurement. For example, if the evaluator counts 16 respirations, acceptable recordings range from 14 to 18 breaths per minute.
No, avoid mentioning respiration counting directly. Say you’re “checking vital signs” or “taking your pulse” to prevent breathing pattern changes that compromise accuracy.
Continue counting from your best estimate without obvious restart behaviors. Maintain a professional demeanor while internally managing the count recovery to avoid alerting evaluators.
Only the Headmaster requires verbal “start” and “stop” announcements. NNAAP and Prometric use silent timing with evaluator observation of your 60-second count period.
NNAAP treats respiration as a standalone skill while Prometric maintains separate skill testing. Both require identical ±2 breath accuracy standards and discreet observation techniques.
Respond professionally: “I’m checking your vital signs” or “Making sure you’re comfortable.” Avoid specific breathing references that might alter their natural respiratory pattern.
Ready to Ace Your CNA Exam?
Get everything you need: video guides, practice tests, and detailed study plans