If you’re feeling anxious about catheter care for your CNA skills test, that concern makes complete sense. This intimate procedure requires technical precision under the evaluator’s observation. The reality many students discover is that training materials often don’t match actual testing requirements, creating legitimate confusion about provider-specific protocols.
Students consistently encounter differences between what they learned in class and what testing providers actually evaluate. Understanding these protocol differences can transform your confidence from uncertainty to competent preparation.
This guide provides comprehensive catheter care guidance for both male and female patients, addresses performance anxiety, and clarifies exactly what each major testing provider requires.
What CNAs Need to Know About Catheter Care Requirements
Testing providers differ in their catheter care protocols because they emphasize different aspects of infection prevention. These variations aren’t arbitrary – they reflect legitimate approaches to comprehensive care.
The Training vs Testing Reality Gap
Working CNAs often find that the biggest challenge isn’t the technical skill itself, but understanding which specific requirements their testing provider emphasizes. One student shared: “I failed my state exam today and failed catheter care. My failure was in cleaning the labia during catheter care. I reviewed my textbook… Nowhere in the catheter care does it acknowledge cleaning the labia.”
This confusion highlights a critical gap between generic training materials and provider-specific testing standards. NNAAP treats catheter care and perineal care as separate skills, while Prometric integrates them.
Why Proper Technique Matters Beyond Testing
Current CAUTI prevention research emphasizes why your technique matters for patient safety. Recent CDC data shows:
- Acute care hospitals achieved CAUTI SIR of 0.62 (38% below baseline) in 2023
- Inpatient rehabilitation facilities saw increases (SIR 1.120, up 8%)
- Each catheter day adds approximately 3-7% risk of CAUTI or bacteriuria
When healthcare teams improved bundle compliance from 84% to 93% reliability, some units saw CAUTI rates drop to zero. Your technique as a CNA contributes directly to these prevention efforts.
Master This Skill With Expert Video Guides
Join 6,000,000+ students who passed with Mometrix’s proven study system
Get Instant Access →Complete Catheter Care Procedure: Male & Female
Follow these numbered steps for confident, competent catheter care that meets all testing provider requirements.
Universal Preparation (Steps 1-3)
1. Perform hand hygiene and gather supplies
- Collect soap, warm water, washcloths, towels, clean gloves, and a protective pad.
- Check the water temperature feels comfortably warm
- Testing insight: All providers require temperature verification
2. Provide privacy and explain the procedure
- Close curtains or doors completely
- Tell the patient what you’ll be doing and why
- Testing insight: Communication demonstrates respect and professionalism
3. Position the patient and apply protective padding
- Help the patient lie comfortably with knees slightly apart
- Place a waterproof pad under the buttocks
- Testing insight: Proper positioning prevents contamination and maintains dignity
Female Catheter Care (Steps 4-7)
4. Don clean gloves and expose the necessary area only
- Put on clean gloves before any patient contact
- Uncover between the hip and the knee while keeping the rest of the body draped
- Testing insight: Minimal exposure maintains patient dignity
5. Provider-specific cleaning requirements
For Prometric testing: Clean the labia first using a soapy washcloth and wiping it front to back. Use a clean section of cloth for each stroke.
For NNAAP/Headmaster: Focus on the catheter area only (labial cleaning is a separate skill).
Testing insight: Know your provider – this difference causes many test failures
6. Clean the catheter insertion area and tubing
- Hold catheter near urethral opening with one hand (prevents tugging – CRITICAL)
- Use your other hand with a soapy washcloth to clean 3-4 inches of tubing
- Move away from the body only, using a clean cloth section for each stroke
- Testing insight: Direction and contamination prevention are critical elements
7. Rinse and dry thoroughly
- Use a clean, damp washcloth (no soap) to rinse the same area
- Pat dry gently with a clean towel
- Testing insight: Complete rinsing prevents skin irritation
Male Catheter Care (Steps 4-7)
4. Position and drape appropriately
- Don clean gloves before patient contact
- Expose only the necessary genital area
- Testing insight: Cultural sensitivity about gender-appropriate care may apply
5. Address foreskin considerations if applicable
- For uncircumcised patients, gently retract the foreskin if needed
- Access the urethral opening carefully
- Testing insight: Gentle technique prevents patient discomfort
6. Clean the catheter and the surrounding area
- Hold catheter steady near urethral opening (prevents tugging – CRITICAL)
- Clean 3-4 inches of tubing away from the body
- Use a clean cloth section for each stroke
- Testing insight: Same technique as female care, adapted for anatomy
7. Complete care properly
- Return the foreskin to its normal position if retracted
- Rinse and dry the area thoroughly
- Testing insight: Foreskin replacement prevents circulation problems
Universal Completion (Steps 8-10)
8. Check drainage system positioning
- Ensure no kinks or dependent loops in tubing
- Confirm the drainage bag is below the bladder level and off the floor
- Testing insight: Proper positioning prevents backflow and infection
9. Secure the catheter appropriately
- Check that the catheter is secured to the patient’s leg or abdomen per policy
- Verify that securement prevents pulling
- Testing insight: Proper securement reduces infection risk
10. Complete care and restore comfort
- Remove soiled linens to the appropriate container
- Empty, rinse, and dry the wash basin
- Remove gloves properly and perform hand hygiene
- Ensure patient comfort with the call light within reach
- Testing insight: Infection control completion demonstrates safe practice
Practice With 600+ CNA Exam Questions
See exactly how this skill appears on the real test
Interactive Catheter Care Skills Checklist
Put your knowledge into practice with our step-by-step interactive checklist. This tool walks you through each critical element based on your testing provider, helping you identify gaps in your preparation and build muscle memory for test day.
Our checklist includes provider-specific requirements, common mistake alerts, and timing guidance based on testing conditions. Use it during practice sessions to ensure you meet all scored elements for your specific state and testing company.
Managing Performance Anxiety During Intimate Care
Feeling nervous about performing catheter care under observation is normal. The intimate nature, combined with testing pressure, creates unique challenges that preparation can address.
Verbalization Strategy
Students consistently report that talking through their actions helps manage anxiety. One community member shared: “Verbalize everything you do on the next test. Like narrate what you’re doing the whole time… that advice saved my butt on catheter care.”
This strategy serves multiple purposes:
- Demonstrates knowledge to evaluators
- Keeps you focused on proper technique
- Reduces anxiety through structured thinking
Breathing and Focus Techniques
Before beginning: Take three slow, deep breaths while reviewing supplies. This brief pause demonstrates thoughtful preparation.
During the procedure: Maintain steady breathing and speak actions aloud: “I’m holding the catheter near the urethral opening to prevent tugging while I clean away from the body.”
Professional Boundary Management
Remember that catheter care is routine healthcare, not intimate personal interaction. Focus on the medical purpose – protecting patients from infection. Understanding that each catheter day increases CAUTI risk by 3-7% helps maintain clinical confidence.
Common Mistakes That Cause Test Failures
Understanding frequent failure patterns helps you avoid critical errors that result in automatic test failure.
Provider Confusion Errors
Labial cleaning misunderstanding: Students trained only on NNAAP may omit labial cleaning with Prometric. Students trained on Prometric may waste time on unnecessary labial cleaning with NNAAP.
Solution: Verify which provider your state uses and understand their specific requirements.
Critical Technical Errors
Contamination through cloth reuse: Using the same washcloth section for multiple strokes introduces bacteria. This is an automatic failure for all providers.
Catheter tugging: Failing to stabilize the catheter while cleaning can cause patient injury. One student noted: “My instructor informed me that I’m supposed to clean the catheter itself” – not the urethra.
Wrong cleaning direction: Moving toward the urethral opening instead of away spreads bacteria toward the insertion site.
Safety and System Errors
Drainage problems: Allowing the bag above bladder level or touching the floor creates backflow risk.
Infection control lapses: Skipping hand hygiene, failing to wear gloves, or contaminating supplies demonstrates unsafe practice.
Testing Provider Comparison: NNAAP vs Prometric vs Headmaster
| Provider | Labial Cleaning | Critical Focus | Scoring Method |
| NNAAP (Credentia) | Separate skill | Catheter tube cleaning | 80% + all critical steps |
| Prometric | Integrated requirement | Comprehensive care | ~75% point system |
| Headmaster | Usually separate | Clean technique | 75% + no missed key steps |
NNAAP Requirements
Focus on catheter tubing care with critical elements, including holding the catheter without tugging and cleaning 4+ inches away from the urethral opening. Water temperature verification and protective padding are required.
Prometric Requirements
Integrates labial cleaning into the catheter care skill. Requires front-to-back cleaning plus catheter tubing care. Emphasizes drainage bag positioning and indirect care behaviors throughout.
Headmaster Requirements
It aligns with the NNAAP approach, often pairing catheter care with handwashing evaluation. Some states include flow verification steps. It emphasizes the ” no missed key steps” rule.
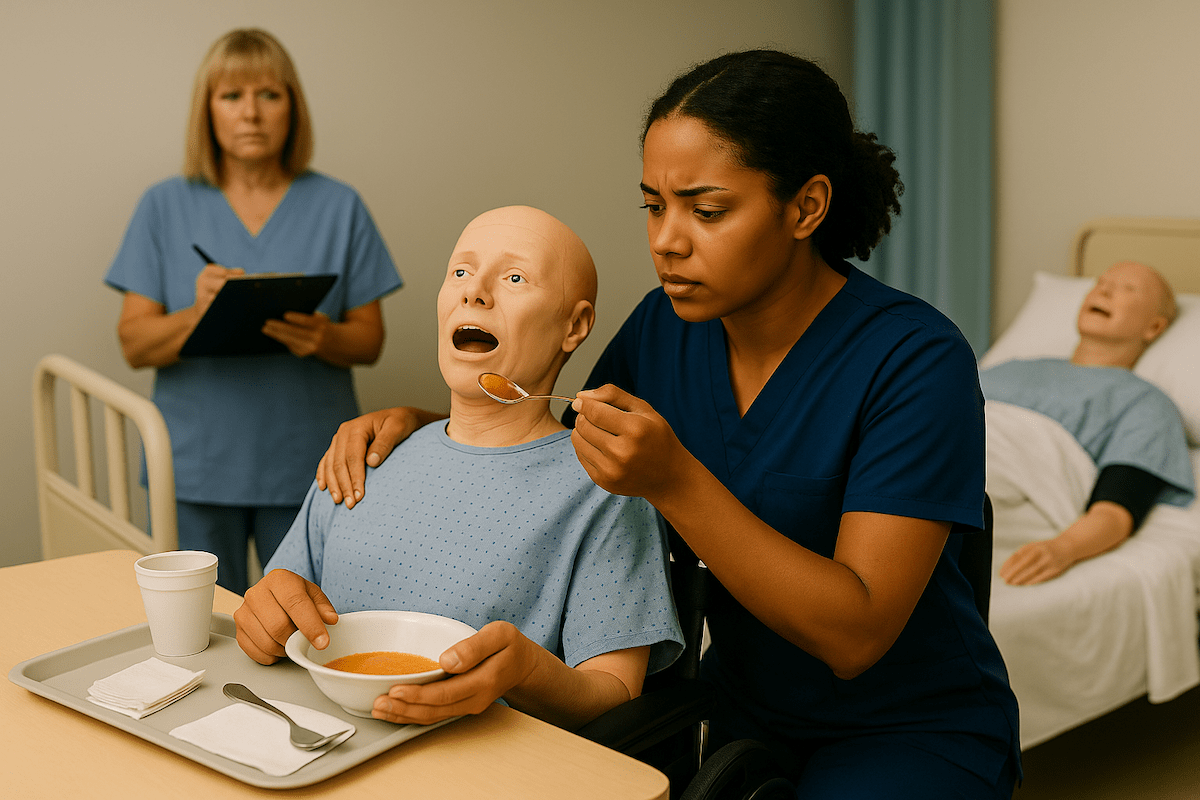
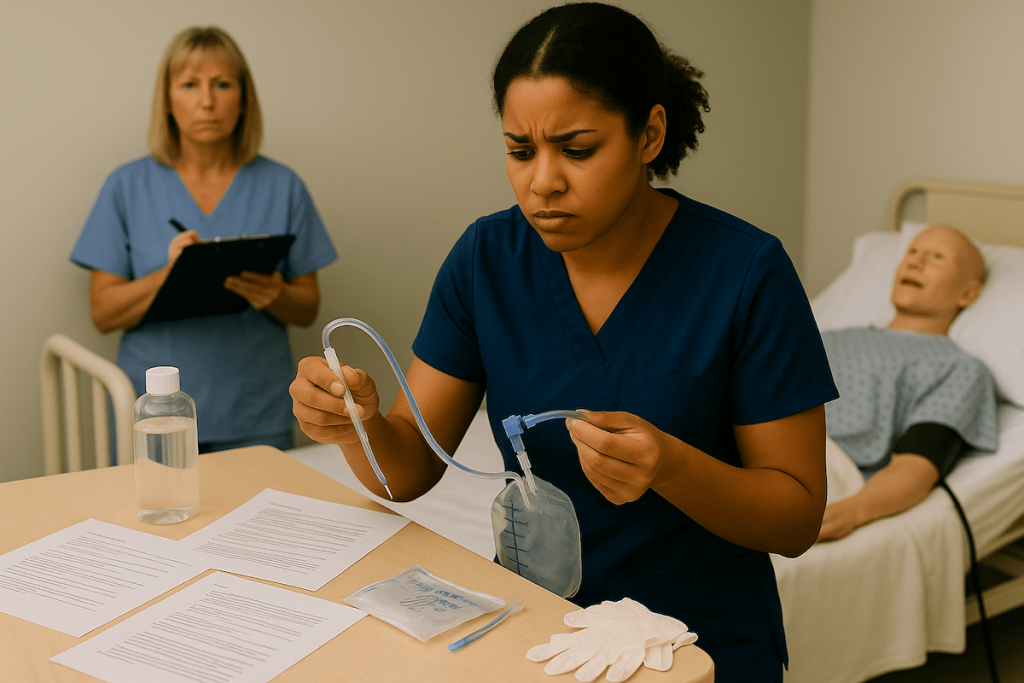
Catheter Care Video Demonstrations
Visual learning reinforces proper technique and builds confidence for hands-on practice. These carefully selected demonstrations show catheter care procedures from multiple angles, helping you understand the spatial relationships and hand positioning that textbook descriptions can’t capture.
Each video demonstrates techniques that align with testing provider requirements. Watch multiple demonstrations to see slight variation approaches that all meet safety and infection control standards.
Catheter Care FAQ for CNA Students
Both require cleaning the catheter tubing away from the insertion site using clean cloth sections for each stroke. Female care may include labia cleaning, depending on your testing provider. Prometric requires it as part of the integrated skill, while NNAAP tests perineal care separately. Male care requires gentle foreskin retraction if uncircumcised, cleaning around the glans and catheter site, and then replacing the foreskin to its natural position after cleaning.
This depends entirely on your testing provider, as each has different skill integration approaches. Prometric integrates labia cleaning as part of catheter care skill, NNAAP tests perineal care separately from catheter care, while Headmaster focuses primarily on catheter tubing cleaning. Check your state’s testing provider before exam day to avoid the confusion that causes many test failures.
Contact your state’s CNA registry or check your testing appointment confirmation emails for the provider name. Key examples include California using both Credentia in the North and Headmaster in the South, Texas using Prometric as of 2023, and Michigan switching to Headmaster in 2021-2022. Provider transitions happen regularly, so verify current requirements rather than relying on older information.
This creates backflow risk and a potential infection pathway that all providers consider a serious safety error. Some providers score this as an automatic failure, while others assign significant point deductions, but all recognize it as demonstrating poor understanding of infection control principles. Always maintain the bag below bladder level during care and when positioning the patient afterward.
Daily catheter care is standard in most facilities, with additional care provided after soiling or as needed based on the patient’s condition. Testing evaluates your technique quality rather than care frequency, demonstrating proper infection control principles and patient dignity during the procedure. Understanding the rationale behind the appropriate technique helps you perform confidently under observation.
Report immediately to the nurse any signs, including cloudy urine, pungent odor, blood in urine, fever, or patient complaints of pain around the insertion site. CNAs observe and report rather than diagnose, but prompt communication about these changes can prevent serious complications. Document your observations clearly and follow your facility’s protocols for urgent notifications.
Specific errors cause immediate failure regardless of how well you perform other technique elements. These critical failures include contaminating sterile areas, causing patient harm, missing essential safety steps, or demonstrating a fundamental misunderstanding of infection control principles. Provider-specific critical elements vary slightly, but all emphasize maintaining safety and sterility throughout the procedure.
Ready to Ace Your CNA Exam?
Get everything you need: video guides, practice tests, and detailed study plans