If you’re feeling anxious about feeding a resident during your CNA skills test, that concern reflects exactly the kind of caring attitude that makes great CNAs. The responsibility of safely assisting someone with eating does carry real weight – aspiration pneumonia affects up to 30% of nursing home residents and carries serious health risks. Understanding the specific requirements for your testing provider while mastering proper safety techniques can transform that anxiety into confident competence.
The confusion many students experience about feeding requirements often stems from conflicting online advice and provider differences. Some sources incorrectly state that gloves are required, while others provide generic guidance that doesn’t match actual testing protocols. This comprehensive guide resolves those inconsistencies using official documentation from NNAAP, Prometric, and Headmaster testing providers, combined with current safety guidelines from CMS and healthcare education research.
Essential CNA Requirements for Safe Feeding Assistance
Students often ask about gloves because the guidance seems contradictory across different sources. Working CNAs often describe the dual nature of feeding assistance: “you’re providing foodservice and nursing care.” This perspective appears frequently in CNA discussions: “both of these things call for gloves, for your benefit and the person you’re feeding.”
Official Testing Requirements:
- No gloves required – NNAAP, Prometric, and Headmaster protocols don’t mandate gloves for feeding
- Hand hygiene is essential – Thorough washing is required for both the CNA and the resident before and after meals
- Focus on cleanliness – Proper sanitation prevents contamination without glove dependency
However, community members express practical concerns: “Do you want someone else’s bare hands in your food, even if they washed them,” which reflects valid thinking about infection control in real practice settings. The distinction matters because testing evaluators follow official checklists that don’t penalize students for wearing gloves, but don’t require them either.
Program directors consistently reference CMS guidelines that show feeding assistance falls outside exposure-prone procedures requiring gloves, provided proper hand hygiene protocols are followed. Understanding why safety protocols exist helps build confidence more than memorizing steps alone.
Critical Safety Context:
- 40% of nursing home residents have some degree of dysphagia (difficulty swallowing)
- 31% mortality rate for aspiration pneumonia in elderly patients
- 18-30% of nursing home pneumonias are aspiration-related
- 75% of choking incidents are preventable with proper supervision
These statistics explain why positioning requirements and swallowing monitoring receive such emphasis in testing protocols. The mortality data provides important context without creating fear – it helps students understand that feeding skills represent genuine patient safety responsibilities, not just testing hurdles.
Master This Skill With Expert Video Guides
Join 6,000,000+ students who passed with Mometrix’s proven study system
Get Instant Access →Step-by-Step Feeding Technique for CNA Skills Testing
Students consistently report this testing experience: “I freeze up when the evaluator watches me feed someone – it’s different than practice.” This practical reference guide provides action-focused steps you can follow during practice and recall during testing.
Master CNA feeding assistance skills testing with this 16-step guide used by 12,000+ successful test candidates. Prevents aspiration risks and ensures compliance across NNAAP, Prometric, and Headmaster testing providers.
- Identify Self and Greet Resident by Name
Introduce yourself by name and address the resident by their preferred name. Evaluators score communication from the first contact across all testing providers.
- Wash Hands Thoroughly
Perform proper handwashing technique for 20+ seconds. All providers require this step as it demonstrates essential infection control knowledge and prevents automatic failure.
- Explain the Procedure to Resident
Clearly describe what you will be doing during the feeding assistance. This demonstrates respect for resident rights and dignity, which evaluators score consistently.
- Provide Privacy Protection
Close curtains, screen, or door to ensure privacy during care. This shows understanding of professional boundaries and patient rights requirements.
- Check Diet Card and Verify Resident Identity
Ask resident to state their name and compare it to the meal tray card. This critical safety step is required by NNAAP and Headmaster testing providers.
- Position Resident Upright at 75-90 Degrees
Raise the head of the bed or assist resident to chair in upright position. This is the most critical safety step – wrong positioning equals automatic failure due to aspiration risk.
- Position Yourself at Resident’s Eye Level
Sit in a chair facing the resident to maintain proper communication technique. This demonstrates professional interaction skills that evaluators specifically assess.
- Place Meal Tray Within Resident’s View
Position tray on overbed table or accessible surface where resident can see food. This maintains resident involvement in the feeding process.
- Help Resident Clean Hands
Use hand wipes or assist with washing hands before eating. All providers require this infection control step to prevent contamination during meals.
- Offer Clothing Protection
Place napkin or clothing protector if resident desires. Required by Prometric and Headmaster; optional for NNAAP testing.
- Describe Foods and Ask for Preferences
Tell resident what’s on the tray and ask what to eat first. This shows respect for autonomy and demonstrates effective communication skills.
- Feed Appropriate Bite Sizes Using Spoon
Offer small bites, describe contents, and wait for complete swallowing before next bite. This safety technique is closely monitored by all evaluators.
- Offer Fluids Regularly
Provide fluids at least once (NNAAP) or every 2-3 bites (Prometric). Provider-specific requirements directly affect scoring on this step.
- Monitor for Swallowing Problems Continuously
Watch for coughing, wet voice, food pocketing, or distress signs. This demonstrates safety awareness and professional judgment that prevents aspiration.
- Complete Post-Meal Care
Clean mouth and hands, remove protector, maintain upright position, and place call light within reach. This final safety check ensures resident comfort and access to help.
- Document Intake if Required by Provider
Record food percentage and fluid mL within accuracy limits. Required by Prometric and Headmaster testing providers; not required by NNAAP.
Key Testing Success Tips:
- Position the resident upright BEFORE offering any food – this is the most critical safety step
- Understand your provider’s specific requirements (clothing protector, documentation, identity verification)
- Focus on resident communication throughout to show a caring attitude
- Remember, 30-minute post-meal upright positioning prevents aspiration
Preventing Aspiration During Feeding Assistance
Clinical experience reveals that CNAs who recognize early warning signs prevent most serious aspiration incidents before they escalate. This concern appears regularly in student forums: “Nobody taught me what to do if someone starts choking during my skills test.” Understanding both recognition and response protocols builds the confidence needed for safe practice.
Recognition Signs of Swallowing Difficulty:
- Coughing or throat clearing during or after swallowing – even subtle sounds indicate potential airway involvement
- Wet, gurgling voice after eating or drinking – suggests liquid or food particles near the vocal cords
- Food pocketing in cheeks or drooling – shows difficulty managing food in the mouth
- Facial expressions of distress – panicked looks, watery eyes, or sudden stopping mid-meal
Students often miss subtle signs because they focus on completing feeding steps rather than continuous monitoring. Program directors notice that CNAs who understand these indicators provide more attentive assistance throughout their careers, catching problems before they become emergencies.
When any of these signs appear, stop feeding immediately and assess the situation. If the resident can cough forcefully, encourage them to “cough it out” while staying close to monitor. Never give water to someone who’s coughing from food – this can worsen aspiration by washing food particles deeper into the airway.
Emergency Response Protocol:
- Call for help immediately – use the call bell or shout for a nurse
- Keep the resident upright – don’t lay them down
- Clear severe obstruction using the Heimlich maneuver if trained, and the resident cannot speak, cough, or breathe
- Begin CPR if the resident becomes unresponsive
- Document the incident thoroughly after the crisis resolves
Many CNAs report feeling unprepared for choking emergencies during testing situations. The key lies in understanding your scope of practice – you’re expected to recognize problems quickly and respond appropriately, not to manage complex medical emergencies alone.
Studies show that 75% of choking incidents are preventable with proper supervision and technique. This statistic empowers rather than frightens – it means your careful attention to positioning, bite size, and swallowing monitoring makes a genuine difference in resident safety.
Practice With 600+ CNA Exam Questions
See exactly how this skill appears on the real test
Feeding Assistance Practice Checklist
Practice your feeding assistance technique with our interactive checklist that tracks your progress through each required step. Download the PDF version to use during your study sessions and bring to clinical practice for quick reference during skills preparation.
Managing Feeding Performance Under Skills Test Observation
Students consistently report this testing experience: “I freeze up when the evaluator watches me feed someone – it’s different than practice.” The artificial nature of testing environments can disrupt even well-practiced techniques, but understanding why this happens helps overcome performance anxiety.
Testing psychology differs from clinical practice because you’re simultaneously caring for a resident and demonstrating competency to an evaluator. Many successful test-takers report that provider-specific preparation eliminated their anxiety about remembering requirements. They focused on understanding rather than memorizing, which prevented mental blanks under pressure.
The resident in your skills test may be a volunteer who doesn’t actually need feeding assistance, creating an unusual dynamic. They might eat independently or provide feedback differently than residents with genuine swallowing difficulties. Maintaining your professional approach regardless of the resident’s actual capabilities shows evaluators your commitment to proper technique.
Mental Preparation Strategies:
- Practice the complete sequence until positioning and safety checks become automatic
- Understand the reasoning behind each step to prevent confusion under pressure
- Rehearse recovery from minor mistakes – evaluators expect human responses, not robotic perfection
- Focus on resident communication throughout – this maintains your caring focus despite testing stress
Experience shows that students who grasp aspiration risks perform more confidently because they understand the genuine importance of their actions. The testing environment becomes less artificial when you remember that these skills protect real people in your future career.
Testing Provider Requirements: NNAAP vs. Prometric vs. Headmaster
Students often express frustration: “Each testing company wants something different – wish someone explained the differences.” Our analysis of official testing protocols reveals distinct variations that affect preparation and testing success.
| Testing Provider | Hand Hygiene | Clothing Protection | Identity Check | Documentation |
|---|---|---|---|---|
| NNAAP | After completion | Not required | Diet card + verbal | None required |
| Prometric | Standard precautions | Mandatory napkin/protector | Greeting by name | Intake % + mL |
| Headmaster | Before AND after | Mandatory protector | Diet card + verbal | Intake % + mL |
NNAAP Protocol Focus: The streamlined approach emphasizes core safety without additional documentation. Hand hygiene occurs after skill completion, and no clothing protector appears on the checklist. Students testing with NNAAP can focus entirely on positioning, safe feeding technique, and post-meal care without worrying about intake calculations.
Prometric Differences: The clothing protector requirement and intake documentation distinguish Prometric testing. Students must estimate consumption percentages and fluid amounts within 25% accuracy, adding a mathematical component to the skill. The emphasis on eye-level positioning and frequent fluid offerings (every 2-3 bites) creates a more detailed interaction pattern.
Headmaster Specifications: The most comprehensive requirements include hand hygiene at both skill beginning and end, making infection control more prominent throughout the process. State-specific variations mean students should review their particular state’s handbook, as some details differ between locations.
All providers share core safety priorities: proper positioning, identity verification, safe feeding pace, and post-meal upright positioning. The differences lie in documentation requirements and specific procedural details that won’t affect resident safety but do influence testing success.
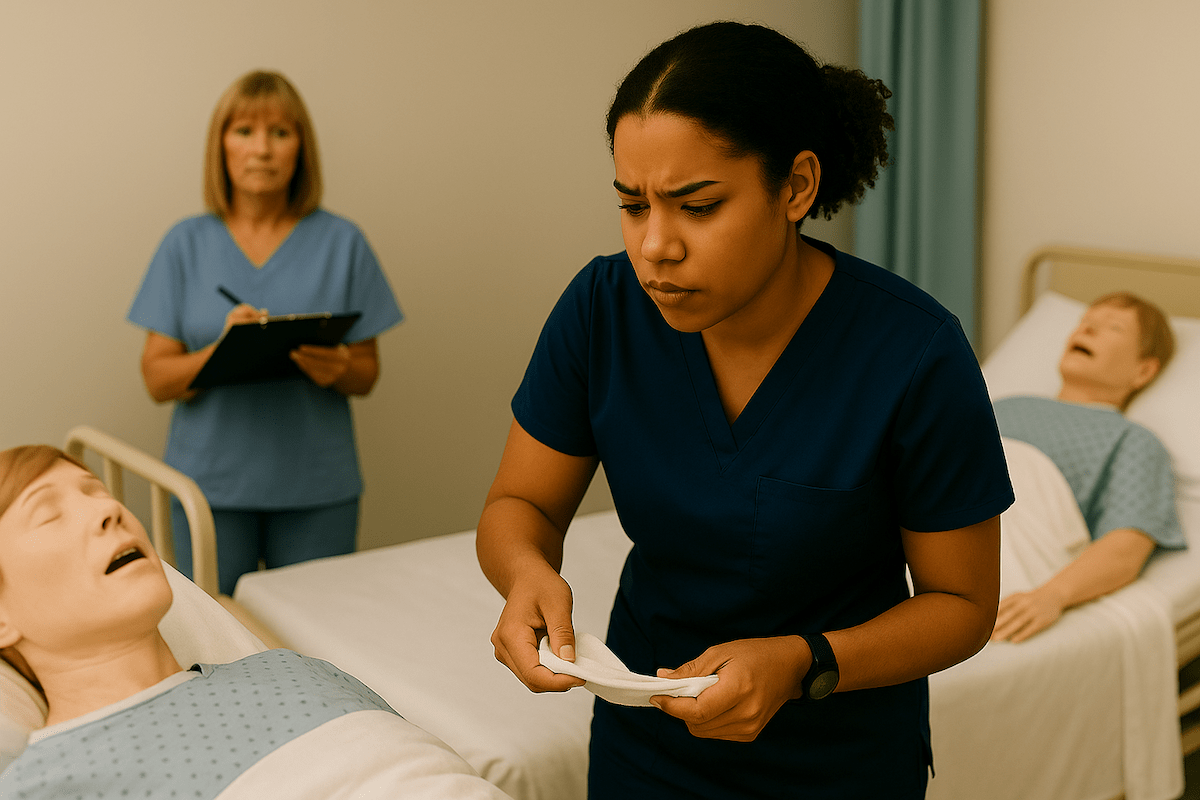
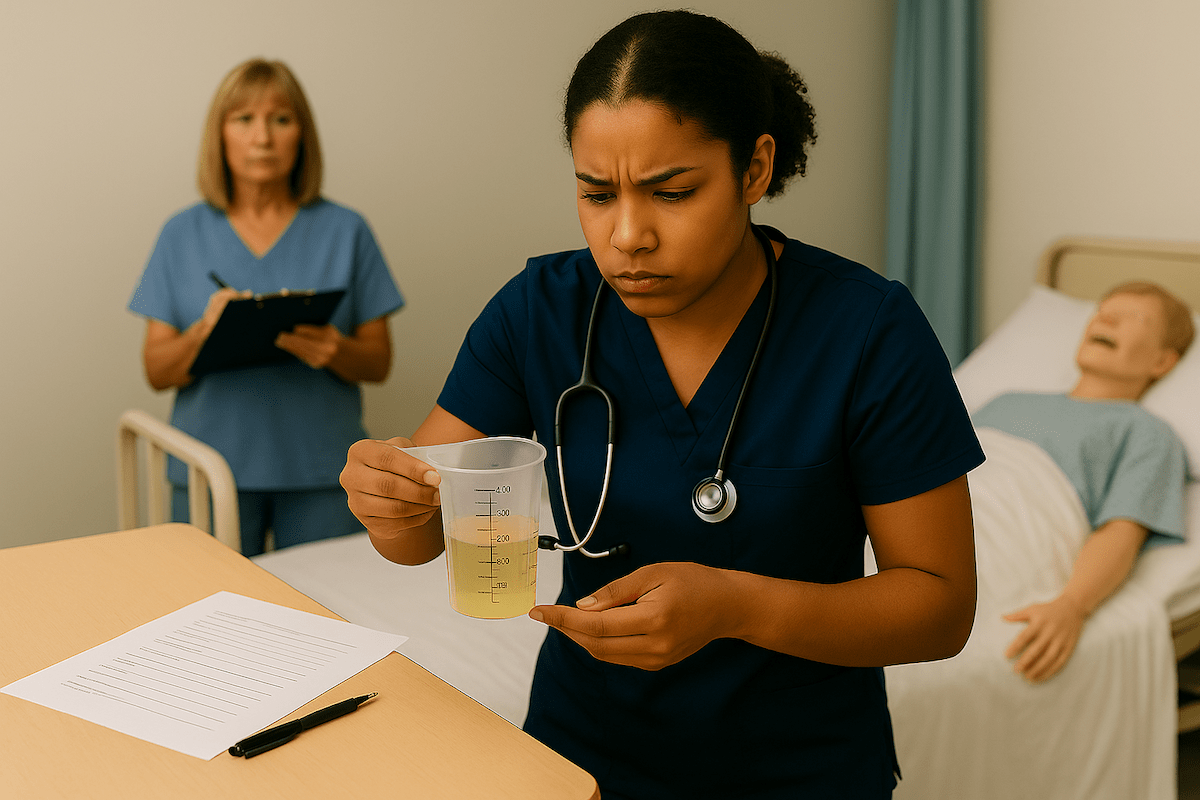
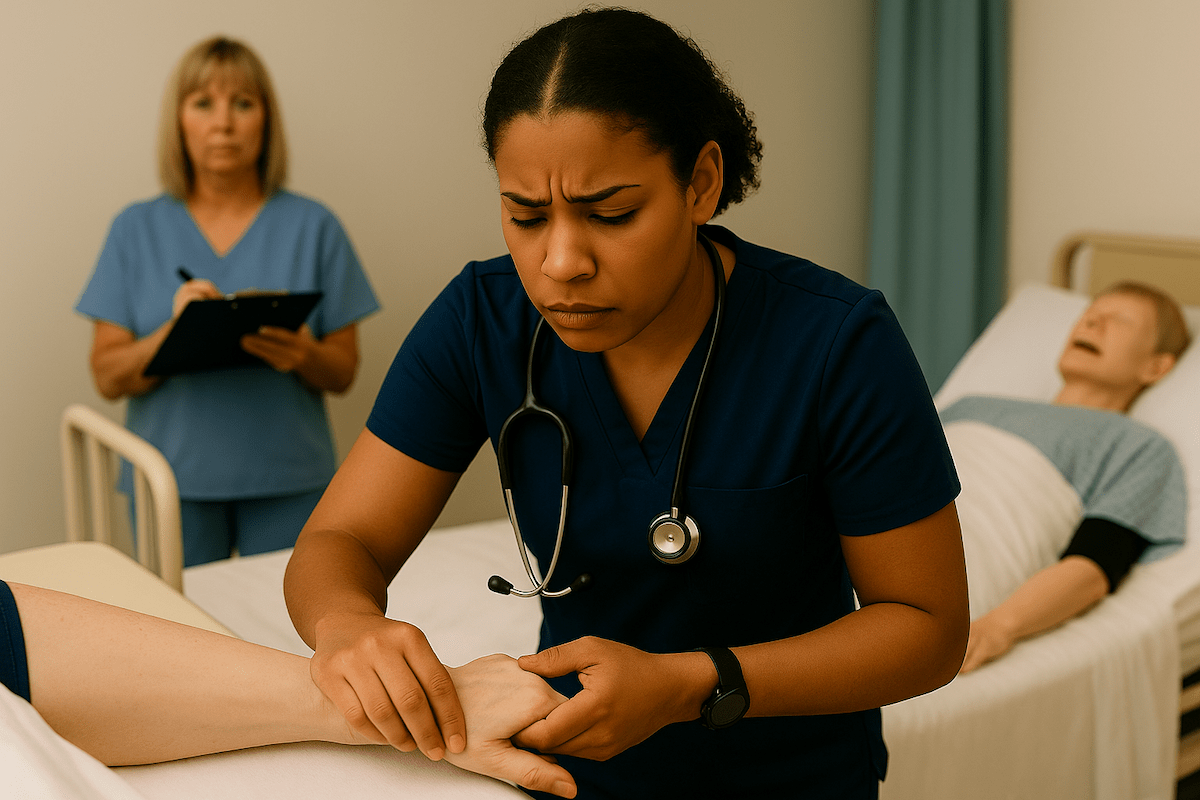
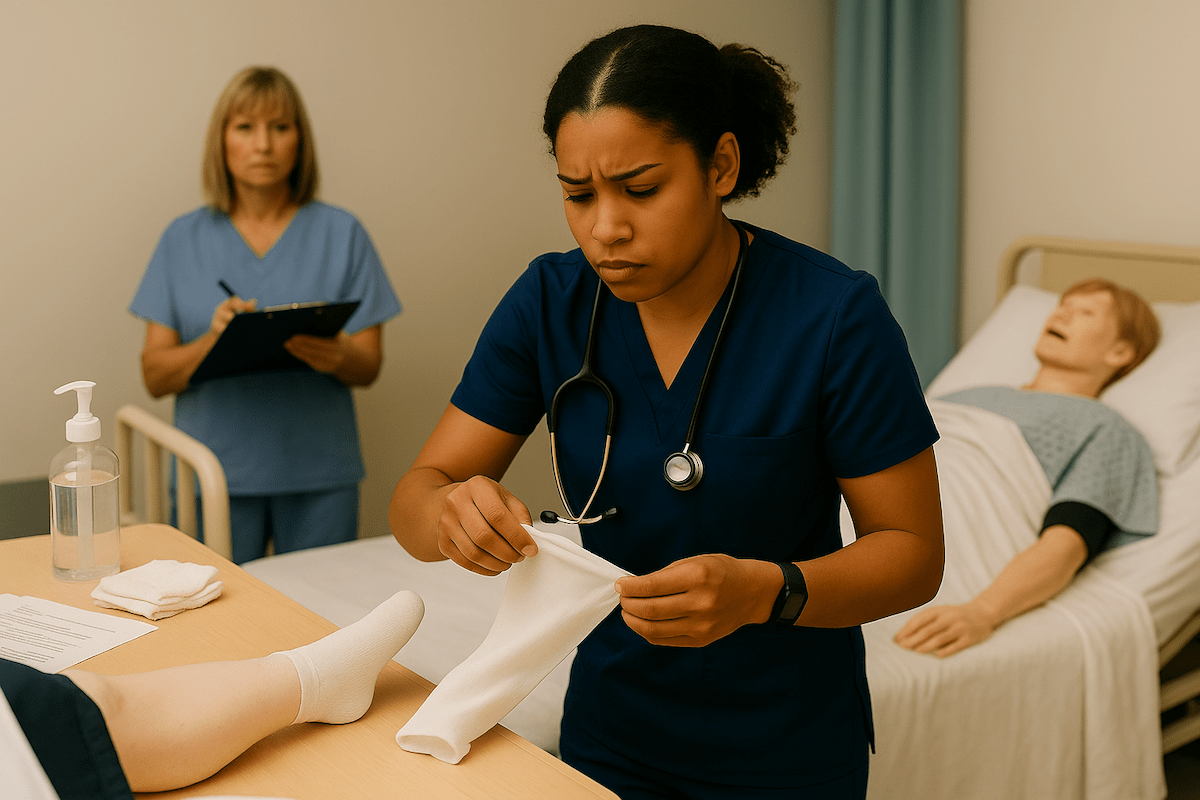
Feeding Assistance Videos
Watch experienced CNAs demonstrate proper feeding techniques in these educational videos from nursing programs and healthcare educators. These visual examples help reinforce the step-by-step procedures and show proper body mechanics, positioning, and communication techniques in real-world settings.
Frequently Asked Questions
Official testing protocols from NNAAP, Prometric, and Headmaster do not require gloves for feeding assistance. Hand hygiene for both CNA and resident provides adequate infection control for this non-exposure-prone procedure.
Residents must be positioned at 75-90 degrees upright before feeding begins. This positioning uses gravity to prevent food from entering the airway and reduces aspiration risk significantly.
Prevention involves proper positioning, offering small bites, ensuring complete swallowing before the next bite, providing fluids regularly, and continuous monitoring for signs of difficulty, such as coughing or a wet voice.
Stop feeding immediately, call for help, keep the resident upright, and assist with airway clearance if trained and the situation requires it. Document the incident thoroughly after the emergency is resolved.
Residents should remain upright for at least 30 minutes after meals to prevent aspiration of any food that might reflux. This positioning completes the safety protocol that begins with proper meal setup.
While all providers emphasize core safety principles, they differ in documentation requirements (intake recording), clothing protection mandates, and specific procedural details that affect testing success but not patient safety.
Ready to Ace Your CNA Exam?
Get everything you need: video guides, practice tests, and detailed study plans