If you’re feeling anxious about mastering indirect care for your CNA skills test, that response makes complete sense. These protocols require precision under evaluator observation, and many students worry about failing due to seemingly basic oversights.
The encouraging reality is that 81.8% of CNA candidates pass on their first attempt when they understand exactly what evaluators are looking for. One student shared, “I thought I knew indirect care until the evaluator watched every move I made.”
What Is Indirect Care and Why Does It Matter for CNAs
Indirect care refers to all the supportive practices surrounding your hands-on skills. These include communication, infection control, safety measures, and dignity protection that should occur with every procedure.
Testing providers evaluate these behaviors separately from technical skill performance. Lapses here contribute significantly to the 18% of candidates who don’t pass on their first attempt.
Why These “Basic” Skills Matter So Much
Working CNAs often express surprise at how much indirect care matters in real healthcare settings. These protocols prevent about 388,000 health-related deaths annually.
The distinction from direct care helps clarify test preparation:
- Direct care: The hands-on procedure itself (taking vital signs, giving bed baths, helping with mobility)
- Indirect care: Everything else that happens during patient interaction
Testing providers have emphasized indirect care evaluation more strongly since COVID-19. Enhanced Barrier Precautions and updated infection control standards now appear across all major testing platforms.
Master This Skill With Expert Video Guides
Join 6,000,000+ students who passed with Mometrix’s proven study system
Get Instant Access →The 4 Essential Components of CNA Indirect Care
Understanding indirect care becomes manageable when you break it into four systematic components that apply to every skill:
1. Communication and Explanation
Greet residents by name, introduce yourself, and explain each step of care before and during procedures. Students often rush this component under test pressure, but evaluators specifically watch for respectful, clear communication throughout your interaction.
2. Infection Control Practices
Hand hygiene represents the most critical element here. Healthcare research shows only 17% compliance in actual nursing home settings.
For testing, this means:
- Washing hands at designated times
- Using gloves appropriately
- Following proper contamination prevention throughout procedures
3. Privacy and Dignity Protection
Pull curtains or close doors, use respectful language, keep residents appropriately covered, and ask about preferences. Many students underestimate how carefully evaluators observe these respectful care practices.
4. Environmental Safety
Check bed positioning, call light placement, wheelchair locks, and equipment safety. Testing data shows safety oversights like leaving beds elevated or call lights out of reach rank among the most common failure points.
Program directors consistently tell us that students who understand the reasoning behind each component perform more confidently than those who simply memorize checklists.
Common Indirect Care Mistakes That Cause Test Failures
Understanding exactly what causes failures helps transform anxiety into systematic preparation. Here are the most documented patterns from testing provider data:
Hand Hygiene Lapses
Students frequently wash their hands only at the very end of care, then continue touching the patient or documentation. This invalidates handwashing according to evaluators.
What to do instead: Follow the specific hand hygiene timing outlined in your state’s testing guidelines. Most require handwashing both before initial contact and after completing care.
Glove Removal Errors
A common violation involves declaring a skill “finished” while still wearing contaminated gloves. Students also fail by removing gloves incorrectly, causing self-contamination.
What to do instead: Remove gloves without touching the outside surface, then immediately perform hand hygiene before touching anything else.
Safety Oversights That Create Critical Failures
Testing providers cite these as immediate failure points:
- The bed was left in an elevated position after care
- Call light placed out of the resident’s reach
- Wheelchair or bed wheels are unlocked during transfers
- Equipment left in unsafe positions
What to do instead: End every skill with a systematic safety check. Lower the bed, position the call light, lock wheels, and ensure the resident’s environment is safe.
Privacy Violations During Care
Evaluators document failures when students:
- Don’t pull curtains or close doors during personal care
- Use inappropriate casual language (“honey” instead of the resident’s name)
- Leave residents improperly covered during procedures
- Forget to knock or announce before entering
What to do instead: Treat privacy as automatic. Pull the curtain first, keep residents covered, and use respectful formal address throughout care.
Practice With 600+ CNA Exam Questions
See exactly how this skill appears on the real test
Interactive Indirect Care Skills Checklist
Master your indirect care timing with our step-by-step interactive checklist. This tool walks you through each protocol in real-time, helping you build the automatic responses needed for confident testing performance. Practice with different skill scenarios, track your progress, and download the PDF version for offline study sessions.
Real-World Application: Bridging Theory and Practice
Many students feel confused because classroom protocols seem different from what they observe in healthcare settings during clinicals. This theory-practice gap is real, but understanding it helps rather than hinders your test preparation.
Why Workplace Shortcuts Happen
Research shows that 66% of understaffed facilities have more protocol violations compared to 55% of well-staffed facilities. Time pressure and resource constraints cause experienced workers to develop shortcuts.
Students frequently mention seeing CNAs skip handwashing between residents or rush through privacy steps. These observations can create doubt about whether protocols really matter.
The Testing Reality vs. Workplace Reality
Your certification exam evaluates whether you know proper protocols, not whether you can work under staffing pressure. Evaluators expect systematic adherence to every step because:
- Patient safety requires consistent habits – shortcuts in real facilities contribute to infection outbreaks
- New CNAs need strong foundational practices – you’ll adapt to workplace realities after building proper technique
- Legal standards haven’t changed – facilities are still cited for the same violations you’re tested on
Working CNAs often express that strong foundational skills from testing preparation actually help them maintain better practices even under workplace pressure.
Practical Solutions for Common Scenarios
When classroom learning meets workplace constraints, focus on these adaptable principles:
- Time pressure situations: Maintain hand hygiene and safety checks even if other steps get abbreviated
- Equipment limitations: Know alternative approaches while maintaining infection control standards
- Staffing shortages: Prioritize resident safety and dignity even when routines get disrupted
Testing Provider Protocols: NNAAP vs. Prometric vs. Headmaster
Understanding your specific testing provider helps focus preparation on the evaluation approach you’ll encounter:
NNAAP Requirements (Credentia/Pearson VUE)
NNAAP uses standardized evaluation criteria across participating states. Key features include:
- Online written exam options with remote proctoring
- Skills evaluation focuses on critical elements vs. minor variations
- Post-COVID integration of Enhanced Barrier Precautions
States using NNAAP include Florida, Virginia, Pennsylvania, and over 20 others.
Prometric Standards
Prometric emphasizes systematic skill demonstration with attention to:
- Step sequence accuracy during complex procedures
- Consistent indirect care integration throughout skills
- Safety protocol maintenance under observation pressure
Testing documentation warns specifically against leaving beds elevated, failing to provide call lights, and saying you’re “done” before removing gloves.
Headmaster Protocols (D&SDT)
The Headmaster has added mandatory PPE skills post-COVID, including:
- “Donning PPE (gown and gloves) and emptying urinary drainage bag with handwashing”
- Enhanced infection control evaluation criteria
- State-specific protocol variations
States using Headmaster include Ohio, Minnesota, Nevada, and Massachusetts.
Universal Post-COVID Changes
All providers now require:
- Mask wearing during testing (candidates and staff)
- Enhanced cleaning between exam sessions
- PPE demonstration skills in many states
- Updated infection control evaluation standards
Mastering Indirect Care Under Testing Pressure
Test anxiety about evaluation observation is completely normal. Research shows that behavioral performance can change significantly when people know they’re being watched – this affects even experienced healthcare workers.
Memory Techniques for Systematic Protocol Recall
Create consistent patterns you can rely on under pressure:
- Opening routine: Knock, introduce yourself, explain the procedure, ask about comfort or preferences
- During care: Maintain communication, check resident responses, ensure privacy and safety
- Closing routine: Complete hand hygiene, position call light, lower bed, ask about comfort
Building Confidence Through Understanding
Students who understand why each protocol exists perform better than those who memorize steps. For example:
- Hand hygiene timing prevents cross-contamination between residents
- Privacy measures protect dignity and comply with HIPAA requirements
- Safety checks prevent falls and injuries that cause serious harm
What Evaluators Actually Look For
Testing providers train evaluators to focus on critical elements, not perfection. They understand test anxiety and watch for a systematic approach rather than flawless performance.
The goal is to demonstrate safe, respectful care practices that protect residents. Minor nervousness won’t fail you if your systematic approach covers the essential components.
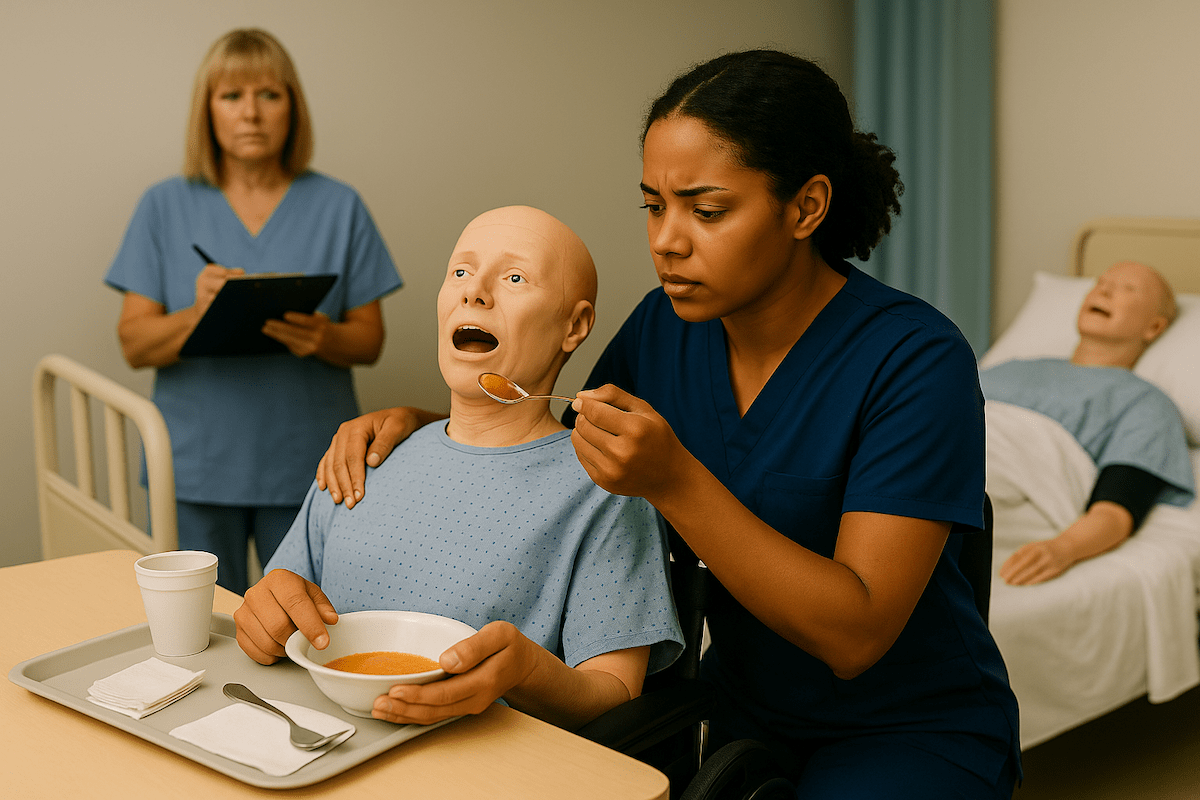
Indirect Care CNA Skill Videos
See proper indirect care protocols demonstrated step-by-step in realistic testing scenarios. These video demonstrations show what evaluators look for during each skill, including common timing mistakes and proper technique under observation pressure.
Watch how experienced CNAs maintain consistent indirect care behaviors while managing testing anxiety, and learn the subtle details that can make the difference between passing and failing your certification exam.
Indirect Care FAQ for CNA Students
Communication and explanation, infection control practices, privacy and dignity protection, and environmental safety are the components that must be demonstrated in every skill on the CNA certification exam.
Research shows common failures include hand hygiene lapses, glove removal errors, safety oversights like leaving beds elevated, and privacy violations. These mistakes can cause test failure even when technical skills are performed correctly.
Post-COVID changes include Enhanced Barrier Precautions, mandatory PPE donning/doffing skills, remote written exam options, and stricter infection control evaluation across all testing providers.
Direct care involves hands-on tasks like taking vital signs. Indirect care includes supportive behaviors during those tasks, such as communication, safety, infection control, and respect for resident rights.
Very strict. Testing provider documentation confirms that indirect care violations can result in automatic skill failure regardless of technical performance quality, emphasizing the critical importance of these protocols.
Yes. Even with perfect technical performance, students can fail individual skills or the entire exam based solely on indirect care violations. This emphasizes how fundamental these behaviors are to safe patient care.
Create systematic checklists for each skill, practice until behaviors become automatic, and focus on the caring purpose behind each protocol rather than just following rules mechanically.
Stay calm and complete the remaining steps properly. Evaluators understand that nerves can affect performance, but consistently demonstrating most indirect care behaviors shows competency.
Ready to Ace Your CNA Exam?
Get everything you need: video guides, practice tests, and detailed study plans