If you’re feeling anxious about hand and foot care for your CNA skills test, that anxiety makes complete sense. This procedure combines technical precision with provider-specific requirements that aren’t always clearly explained. The good news is that understanding exactly what each testing provider expects can transform your nervousness into genuine confidence.
This unified skill demonstrates your competence in infection control, patient safety, and personal care fundamentals that you’ll use daily as a CNA. Program directors notice that students who master both hand and foot care components during training show stronger professional confidence in workplace settings.
What CNAs Need to Know About Hand and Foot Care Requirements
Hand and foot care represents a combined competency that testing providers evaluate as one skill, reflecting the integrated nature of personal care in healthcare settings. Students consistently find that understanding this unified approach reduces testing complexity rather than increasing it.
Why Provider Differences Matter for Testing Success
Testing experiences from CNA students reveal how provider inconsistencies pose unexpected challenges: “For context, I live in the state of GA. I had five skills… I passed all except for foot care, where the proctor indicated I missed one step, which was placing the client’s foot in the basin.”
This evaluation inconsistency highlights why understanding provider protocols matters beyond basic technique memorization. According to current testing provider documentation, NNAAP requires gloves for foot care, while Prometric doesn’t explicitly mandate them. Headmaster testing adds verbalization requirements that other providers don’t use.
Post-COVID Testing Environment Changes
Enhanced sanitizer protocols remain in many states, with provider-specific mask policies still varying by testing site. Current Prometric testing site policies allow mask-optional testing in most locations, while some NNAAP state programs continue requiring medical masks during skills evaluation.
These differences aren’t minor details – they represent critical elements that determine pass or fail outcomes.
Master This Skill With Expert Video Guides
Join 6,000,000+ students who passed with Mometrix’s proven study system
Get Instant Access →Step-by-Step Hand and Foot Care Technique for CNA Testing
Testing providers have structured this skill to evaluate your infection control knowledge, patient safety awareness, and technical competence simultaneously. Experience shows that candidates who understand the reasoning behind each step perform more confidently under an evaluator’s observation.
Hand Care Sequence (Steps 1-8)
1. First, you’ll perform hand hygiene and gather supplies on a clean barrier
- Why it matters: First demonstration of infection control for evaluators
- Supplies needed: Basin, two towels, orangewood stick, emery board, pump lotion
2. Next, you’ll explain the procedure and assess the resident’s hand
- Action: Check for wounds, redness, swelling before beginning
- Why it matters: Shows safety awareness and communication skills
3. Then, you’ll fill the basin with warm water, test the temperature with your wrist/elbow
- Diabetic modification: Skip soaking entirely – go directly to washing
- Why it matters: Temperature safety prevents burns in residents with neuropathy
4. You’ll allow non-diabetic residents to soak for 5-10 minutes
- Headmaster testing: Verbalize “soaking at least 5 minutes” and wait for acknowledgment
- Why it matters: Softens skin and demonstrates provider-specific protocols.
5. Next, you’ll clean under each nail with an orangewood stick
- Action: Wipe tip between nails, discard stick after one resident
- Why it matters: Prevents cross-contamination, shows infection control
6. Then, you’ll file nails straight across with an emery board
- Diabetic rule: File only, never cut
- Why it matters: Cutting exceeds the CNA scope, especially risky for diabetics
7. You’ll apply lotion from the pump dispenser
- Avoid: Between fingers if maceration risk exists
- Why it matters: Prevents container contamination, reduces slip hazards
8. Finally, you’ll clean equipment and perform final hand hygiene
- Why it matters: Completes the infection control cycle that evaluators expect
Foot Care Sequence (Steps 9-15)
9. First, you’ll place the basin on a protective barrier, positioning it for body mechanics
- Why it matters: Prevents contamination, protects your knees and back
- Tip: Adjust position as needed – evaluators understand physical demands
CNAs in the field consistently describe the physical demands: “It is brutal on your knees, little else comes close job-wise. You’re kneeling and bending over all shift to change trash, put on briefs, and do foot care.”
10. Next, you’ll fill the basin with warm water, verify the temperature
- Diabetic caution: Extra temperature care due to reduced sensation
- Why it matters: Prevents burns in vulnerable residents
11. Then, you’ll apply gloves based on testing provider requirements
- NNAAP: Required for foot care
- Prometric: Not explicitly required
- When unsure: Use gloves – shows infection control judgment
12. You’ll wash your feet thoroughly, including between your toes
- Focus areas: Spaces where moisture and bacteria accumulate
- Why it matters: Prevents fungal infections, demonstrates thoroughness
13. Next, you’ll rinse using the evaluator’s preferred technique
- Option 1: Keep foot in basin throughout
- Option 2: Lift foot out for washing, return for rinsing
- Why it matters: Adapts to evaluator expectations while maintaining care quality
This evaluation inconsistency highlights why understanding provider protocols matters: “However, I did place it in the basin to soak and then lifted it to wash and rinse with the washcloths. Her comment on the skill said that I should’ve kept their feet in the basin while washing and rinsing, which is not in their official handbook for the skill.”
14. Then, you’ll dry completely, especially between toes
- Why it matters: Prevents maceration and fungal growth
- Evaluator focus: Thorough drying shows infection prevention awareness
15. Finally, you’ll apply lotion to the top and sole only, and complete the cleanup
- Never: Apply lotion between toes
- Provider variations: Replace sock/shoe if required (Prometric/Headmaster yes, NNAAP typically no)
- Final step: Equipment cleanup and hand hygiene
Quick Reference – Provider Differences
| Provider | Gloves Required | Verbalization | Sock Replacement |
|---|---|---|---|
| NNAAP | Yes for foot care | No | Typically no |
| Prometric | Not explicit | No | Yes, plus shoes |
| Headmaster | Standard precautions | Yes – soak times | Yes |
Practice With 600+ CNA Exam Questions
See exactly how this skill appears on the real test
Interactive Hand & Foot Care Skills Checklist
Practice makes perfect, and our interactive checklist helps you master each step while tracking your progress through the 15-step procedure. This digital tool lets you check off completed steps, note provider-specific variations, and identify areas needing additional practice before your testing day.
Download our comprehensive PDF checklist to take with you during hands-on practice sessions or skills lab time. The printable format includes space for notes, provider-specific reminders, and common mistake warnings to support your preparation wherever you practice.
Managing Evaluator Expectations and Testing Variations
Understanding how evaluators are trained helps you anticipate what they’re looking for during your test. Each testing provider trains their RN evaluators differently, which explains why experiences can vary even within the same state.
Evaluator Training Differences by Provider
NNAAP (Credentia) Evaluators
- Focus on critical elements vs. non-critical steps
- Trained to observe hand hygiene at specific moments
- May allow minor technique variations if safety isn’t compromised
Prometric Evaluators
- Use the standardized Clinical Skills Checklist scoring.
- Florida uses two evaluators (one watches initial handwashing, the other observes skill completion)
- More structured observation with less flexibility for variations
Headmaster Evaluators
- Require scripted acknowledgments for verbalized timing.
- Emphasize embedded hand sanitizer protocols throughout
- RN Test Observers follow state-specific contractor guidelines
Managing Testing Anxiety Under Observation
Many students share similar testing experiences about evaluator pressure. Remember that these professionals want you to succeed – they’re there to verify competence, not create obstacles.
Practical anxiety management:
- Practice verbalizing your actions during training
- Expect evaluators to take notes throughout your performance
- Don’t interpret note-taking as a failure indicator
- Ask for clarification if instructions seem unclear
State-Specific Variations to Know
- Wyoming (Prometric): Hand and nail care isn’t tested as a standalone skill.
- Florida (Prometric): The two-evaluator system affects pacing and observation dynamics.
- Arkansas (Headmaster): Enhanced verbalization requirements for all timing elements
Check your state’s specific testing policies before your exam date, as provider protocols can include local adaptations.
Advanced Safety Protocols for Diabetic Patients and Infection Control
Professional CNAs understand that diabetic residents require modified approaches based on physiological changes that affect healing and sensation. These aren’t arbitrary rules – they reflect evidence-based safety protocols.
Diabetic Patient Modifications
Temperature sensitivity protocols:
- Test the water temperature multiple times during the procedure
- Use lukewarm rather than warm water
- Monitor the resident’s comfort level throughout
Skin integrity protection:
- Never soak hands or feet (increases maceration risk)
- File nails only – cutting requires podiatry referral
- Inspect carefully for any breaks, cracks, or color changes
- Apply lotion to the top and sole only, never between toes
Infection prevention focus:
- Report any redness, warmth, swelling immediately using the SBAR format
- Document all observations in detail
- Understand that minor injuries can become serious quickly
WHO 5 Moments Hand Hygiene Application
- Before resident contact: Initial hand hygiene before gathering supplies.
- Before a clean/aseptic task: Hand hygiene is important before handling clean equipment.
- After body fluid exposure risk: After any contact with potentially contaminated areas.
- After resident contact: After completing all care activities.
- After contact with the resident’s surroundings: After handling bed rails, tables, and call lights
Enhanced Barrier Precautions for High-Risk Residents
Based on current CMS guidelines, nursing home residents with wounds or indwelling devices require a gown and gloves for high-contact care activities, even without formal Contact Precautions.
When to apply Enhanced Barrier Precautions:
- Residents with any open wounds
- Indwelling catheters or feeding tubes
- Recent hospitalizations or antibiotic use
- Known colonization with resistant organisms
Common Mistakes That Cause Hand and Foot Care Test Failures
Understanding failure patterns helps you avoid preventable mistakes that trip up otherwise well-prepared candidates.
Provider Protocol Violations
NNAAP-specific failures:
- Missing required gloves for foot care
- Inadequate hand hygiene timing
- Cross-contamination during equipment handling
Prometric-specific failures:
- Failing to replace socks and shoes when required
- Incorrect water temperature verification
- Missing embedded safety checks
Headmaster-specific failures:
- Not verbalizing required soak times
- Missing RN observer acknowledgment cues
- Inadequate hand sanitizer integration
Cross-Contamination Errors
Students often fail by contaminating clean supplies or reusing single-use items.
Common patterns include:
- Placing clean towels on contaminated surfaces
- Reusing orange sticks between nails
- Double-dipping lotion containers
- Inadequate basin disinfection between uses
Safety Protocol Failures
Diabetic care violations:
- Soaking when contraindicated
- Using hot water temperatures
- Applying lotion between toes
- Attempting nail cutting
Infection control gaps:
- Missing critical hand hygiene moments
- Improper glove removal technique
- Inadequate equipment disinfection
- Poor body mechanics leading to contamination
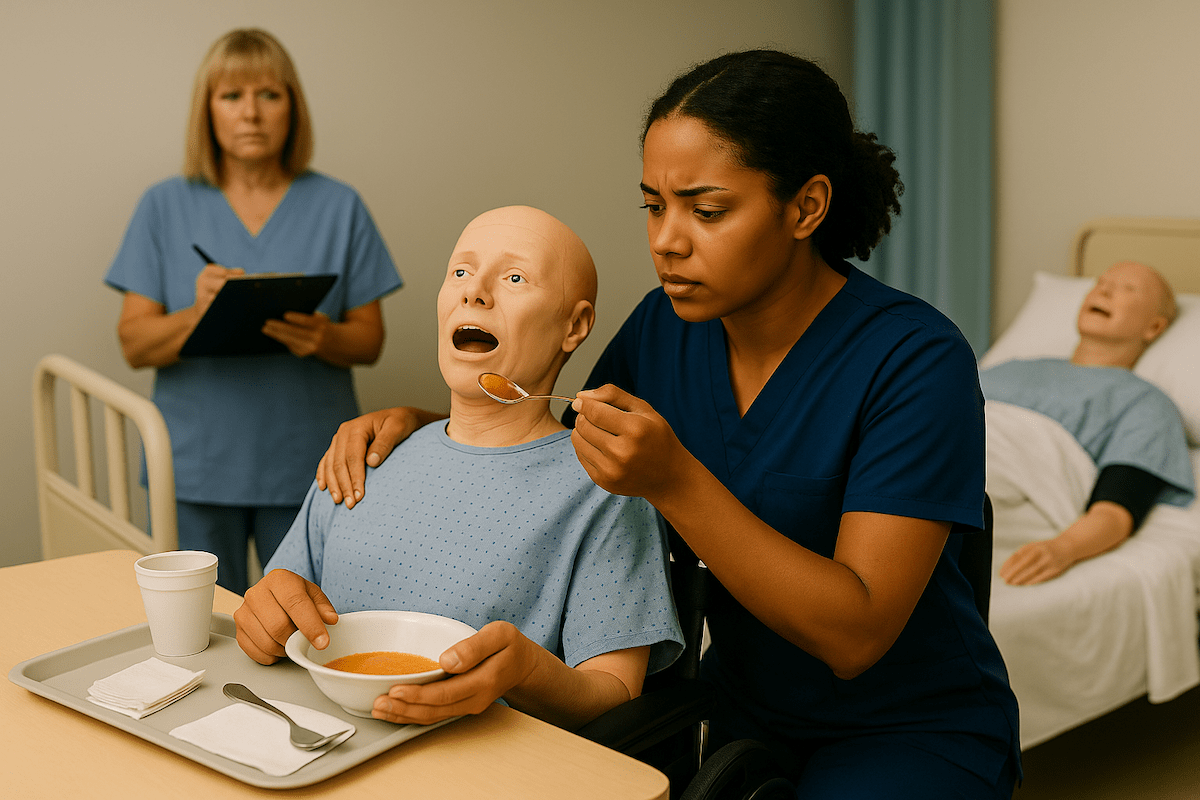
CNA Hand and Foot Care Video Demonstrations
Visual learners benefit from watching hand and foot care techniques demonstrated by experienced CNAs and instructors. These curated video demonstrations show the unified approach, highlighting proper body mechanics and provider-specific variations that prevent testing failures.
Each video reinforces the 15-step procedure while demonstrating the physical positioning and equipment handling techniques that protect you and your patients. Use these demonstrations alongside your hands-on practice to build confidence and muscle memory for testing success.
Hand and Foot Care FAQ for CNA Students
NNAAP requires gloves for foot care, while Prometric doesn’t explicitly mandate them in their checklist. The Headmaster follows standard precaution guidelines. When uncertain, using gloves demonstrates professional infection control judgment without violating any provider’s requirements.
For non-diabetic residents, 5-10 minutes for hands and 5-20 minutes for feet. The Headmaster requires verbalizing soak times and waiting for the RN observer’s acknowledgment. For diabetic residents, skip soaking entirely to prevent skin maceration.
Most facilities restrict nail cutting for diabetic residents to licensed nurses or podiatrists. CNAs typically file nails only, as cutting increases injury risk in patients with poor wound healing and reduced sensation.
Practice both techniques during training. Some evaluators prefer keeping the foot in the basin throughout washing and rinsing, while others allow lifting it out. This inconsistency reflects different interpretations of provider guidelines rather than clear protocol differences.
NNAAP requires gloves for foot care; Prometric emphasizes sock/shoe replacement; Headmaster mandates verbalization of timing. Understanding these differences prevents unexpected failures due to provider-specific expectations.
Stop the procedure and report immediately to the supervising nurse using SBAR format: Situation (wound location and appearance), Background (resident’s risk factors), Assessment (your observations), Recommendation (request immediate nurse evaluation).
Ready to Ace Your CNA Exam?
Get everything you need: video guides, practice tests, and detailed study plans