“Management will gut you like a fish if it means saving face for the state.”
This isn’t paranoia from a disgruntled CNA – it’s survival wisdom from a veteran warning newcomers about the hostile reality of understaffed nursing facilities. And it’s backed by enforcement data: according to NurseJournal.org analysis of National Practitioner Data Bank records, 18,145 adverse actions were taken against nursing licenses in 2021, with 9.7% explicitly involving documentation errors or omissions.
Your CNA license is at risk every shift you work in unsafe conditions. As a CNA, your license authorizes you to provide specific CNA role and responsibilities within defined scope – and defensive documentation protects this authorization when unsafe conditions force you to work outside safe parameters. When state surveyors arrive to investigate a fall, pressure injury, or complaint, your facility won’t protect you. The Department of Health and Human Services Office of Inspector General discovered nursing homes failed to report 43% of falls with major injury to CMS – systematic underreporting proves facilities hide what protects them, not you.
But there’s one thing management can’t erase: the documentation you keep at home.
🛡️ Create Your Documentation in 60 Seconds
HIPAA-compliant templates ready to use – protect your license today
Why Defensive Documentation Is Your Legal Lifeline
Working CNAs face three simultaneous threats that defensive documentation directly protects against: impossible workload standards creating care gaps, coworker neglect you witness but didn’t cause, and facility evidence destruction when state investigations begin.
Your License Is at Risk Every Shift
Veteran CNAs share survival wisdom with newcomers:
“Grow a thick skin. You will get called everything but your name by some residents. Don’t be afraid to stand up to coworkers/nurses politely. Do not let other staff corner you into doing something outside the scope of your license.”
(395 upvotes – Reddit user)
When coworkers pressure you to perform tasks outside your scope, accept unsafe resident ratios, or skip safety protocols, your verbal objection disappears the moment that shift ends. Cornell Law School’s database of federal regulations shows facilities must prevent resident deterioration through adequate care and services under 42 CFR § 483.25 – but when they fail, the CNA providing direct care becomes the scapegoat unless you have contemporaneous documentation proving systemic failure.
Management Won’t Protect You – Documentation Will
As one experienced CNA warns peers:
“Management is not there to protect you and will gut you like a fish if it means saving face for the state. Make sure you document EVERYTHING to cover your ass.”
(Reddit user)
This blunt assessment reflects reality. California facilities investigated by the California Department of Public Health Elder Abuse Advocates paid $2,500 for documenting 28 phantom therapy sessions on days staff weren’t present – investigators cross-referenced documentation with payroll records. Your facility will destroy, edit, or “lose” incident reports that document its liability. That’s why personal backup documentation you keep at home is critical.
Understanding What You CAN vs. CANNOT Document

The biggest barrier preventing CNAs from creating protective documentation is HIPAA confusion. You invested time and money earning your certification through CNA exam and certification standards – defensive documentation protects this professional credential when facilities create conditions that risk your license. You’re not violating privacy laws by documenting unsafe staffing conditions – you just need to know which 18 identifiers to exclude.
The 18 HIPAA Identifiers You Must Exclude
According to the Health and Human Services HIPAA privacy regulations, Protected Health Information includes these specific identifiers:
- Names (patient, relatives, employers)
- Geographic subdivisions smaller than the state
- Dates (birth, admission, discharge, death) except year
- Telephone numbers
- Fax numbers
- Email addresses
- Social Security numbers
- Medical record numbers
- Health plan beneficiary numbers
- Account numbers
- Certificate/license numbers
- Vehicle identifiers and license plate numbers
- Device identifiers and serial numbers
- Web URLs
- IP addresses
- Biometric identifiers
- Full-face photographs
- Any other unique identifying number or characteristic
Notice what’s NOT on that list: staffing ratios, equipment availability, shift timeline, and your objection to unsafe conditions. Documenting “1:20 CNA ratio, 7-11 PM shift, gait belt unavailable” includes ZERO protected health information. The HHS HIPAA whistleblower exception under 45 CFR § 164.512 permits disclosure to health oversight agencies for investigations – you CAN report unsafe conditions to state survey agencies without violating privacy laws.
Objective vs. Subjective Documentation
Professional liability insurers emphasize that objective language protects against claims. NSO (Nurses Service Organization) documentation guidance explains that verifiable facts hold up in investigations while subjective opinions get dismissed.
Objective (Use this): “Assigned 20 residents as sole CNA for 3-11 PM shift. Notified charge nurse J.S. at 3:15 PM that the assignment exceeds safe standards. Request for additional staff denied.”
Subjective (Avoid this): “The facility is dangerously understaffed and management doesn’t care about patient safety.”
The objective version is stronger evidence because investigators can verify assignment sheets, staffing records, and supervisor responses. Your feelings about the situation don’t matter in hearings – provable facts do.
Your Personal CYA File: The Evidence Management Can’t Destroy
Experienced CNAs consistently advise peers:
“Document everything at home for your records…make a copy of the incident report. Nursing homes do not give a flying F about their staff.”
(Reddit user)
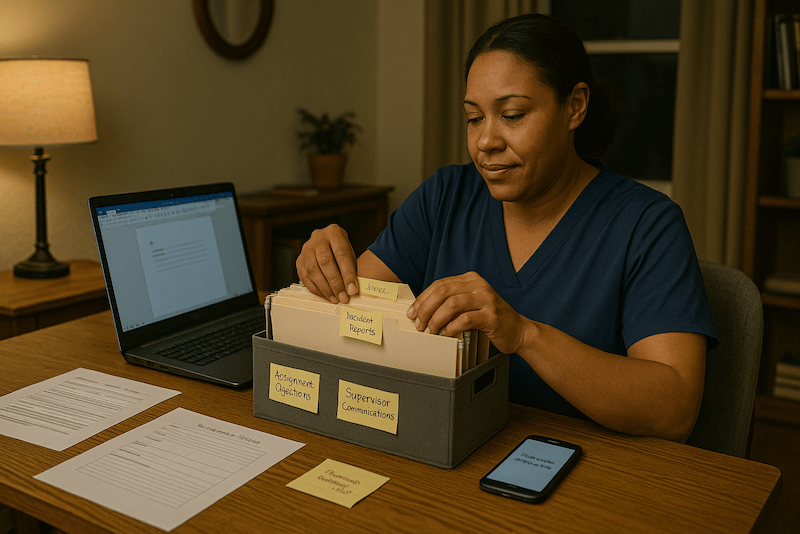
Your personal CYA (Cover Your Ass) file solves the problem of evidence destruction. Facilities can edit EMR records, lose paper incident reports, or claim you never objected – but they can’t access documentation you keep at home in a secure folder.
What to Keep in Your Personal File
- Assignment objection records: Each shift where the ratio exceeded safe standards
- Incident report copies: Falls, injuries, witnessed neglect (with identifiers removed)
- Supervisor communications: Emails, text screenshots showing you reported concerns
- Equipment shortage logs: Dates/times gait belts, lifts, or supplies were unavailable
- Shift notes: Summary of each shift’s staffing, critical incidents, and concerns raised
How Long to Retain Documentation
The National Council of State Boards of Nursing’s guidance on board investigations recommends a minimum of 5 to 7 years. Unlike malpractice lawsuits, which are subject to statutes of limitation, state board investigations can be initiated at any time. Keep records until you’re confident the statute window has closed or you’ve left healthcare entirely.
Organization strategy: Store chronologically by date in labeled folders. When state investigators contact you about an incident from six months ago, you want to locate your contemporaneous documentation in under 60 seconds.
HIPAA-Compliant Documentation Templates for 6 Common Scenarios
Remember the systematic study skills and professional development habits you used preparing for your CNA exam? Defensive documentation requires the same methodical approach. These templates provide exact language you can copy-paste and customize for immediate use. All templates exclude HIPAA identifiers and use objective language that holds up in investigations.
Choose your approach:
- Interactive Generator (60 seconds) – Answer a few questions and get customized documentation ready to save
- Copy/Paste Templates (below) – Browse all 6 scenarios and adapt the template you need
HIPAA-Safe Documentation Generator
Create legally defensible documentation in 60 seconds – Protect your license from facility liability
Preview Your Documentation
Preview Your Documentation
Preview Your Documentation
Preview Your Documentation
Preview Your Documentation
Preview Your Documentation
Scenario 1: Unsafe CNA-to-Patient Ratios
The CMS Payroll-Based Journal system requires facilities to submit quarterly staffing data – creating an official record you can reference when documenting discrepancies between reported and actual staffing.
Scenario 1: Unsafe CNA-to-Patient Ratios
Click to view template and example
Scenario 2: Missing Safety Equipment
Federal regulations under 42 CFR § 483.25 require facilities to provide adequate care that prevents resident deterioration, including necessary safety equipment.
Scenario 2: Missing Safety Equipment
Click to view template and example
Scenario 3: Inability to Complete Assigned Care
Healthcare workers across specialties describe the same impossible reality:
“Last night I was the only RN for 14 patients…My CNAs were stretched just as thin…This isn’t nursing, it’s damage control. I’m documenting assessments I barely had time to perform…”
(1313 upvotes – Reddit user)
When you can’t complete all assigned care due to an impossible workload, documenting “attempted but unable” protects you from neglect findings by establishing systemic failure, not individual negligence.
Scenario 3: Inability to Complete Assigned Care
Click to view template and example
Scenario 4: Witnessing Neglect or Dangerous Situations
CNAs emphasize documentation as professionalism, not tattling:
“At least try, and if they resist/refuse, communicate that to the nurse and document it…The rest is basic civility and professionalism.”
(293 upvotes – Reddit user)
When you witness coworker neglect or dangerous situations, documenting protects both patients and your license. The Oregon Nurses Association guidance on reporting patient condition changes establishes that failure to report patient safety concerns carries disciplinary consequences.
Scenario 4: Witnessing Neglect or Dangerous Situations
Click to view template and example
Scenario 5: Management Refusal to Address Safety Concerns
The National Nurses United ADO (Assignment Despite Objection) guide explains that documenting objections shifts liability from the individual to the facility. Even non-union CNAs benefit from creating assignment objection records.
Scenario 5: Management Refusal to Address Safety Concerns
Click to view template and example
Scenario 6: Patient Falls During Understaffed Shifts
The OIG investigation showing 43% of falls with major injury unreported proves facilities hide evidence. Your documentation should demonstrate you knew proper gait belt ambulation techniques but couldn’t apply them due to unsafe ratios preventing adequate supervision. Your documentation creates the record they won’t.
Scenario 6: Patient Falls During Understaffed Shifts
Click to view template and example
Union vs. Non-Union Documentation Strategies
About 60-70% of CNAs work in non-union facilities and believe that Assignment Despite Objection (ADO) forms don’t apply to them. That’s not true – you can create personal objection records with an identical protective function.
Union ADO Forms
If you’re in a facility with union contracts through organizations like National Nurses United or Massachusetts Nurses Association, use their official ADO forms. These create business records facilities can’t destroy and provide legal framework shifting liability from you to management when they force you to accept unsafe assignments.
Non-Union Personal Objection Records
When you don’t have union ADO forms, create your own assignment objection record using the Scenario 1 template above. The National Labor Relations Board Section 7 protections for concerted activity apply when two or more employees act together for mutual aid. If you and another CNA both document unsafe ratios, that’s protected concerted activity even without a union.
Key distinction: Washington Department of Health patient abandonment guidance clarifies abandonment requires accepting assignment AND severing the nurse-patient relationship without notification. Refusing an assignment BEFORE accepting it is NOT abandonment – it’s a protected safety objection if documented properly.
How to Report Unsafe Staffing Conditions
When personal documentation alone isn’t resolving safety issues, external reporting triggers state investigations. You have multiple pathways depending on anonymity needs and desired investigation speed.
State Health Department Procedures
CMS maintains a national directory of state survey agencies where you file nursing home complaints. Investigation timelines vary dramatically:
- California: 60-day maximum for long-term care complaints, among fastest in nation
- Texas: 1-800-458-9858 hotline Mon-Fri 7am-7pm Central
- Illinois: 1-800-252-4343 hotline available 24/7, most accessible intake system
- New York: 1-888-201-4563 centralized intake
- Florida: Anonymous complaint portal strategic for non-union CNAs in weak protection states
Tennessee’s 2024 Annual Nursing Home Inspection Report shows 53.3% substantiation rate – 1,354 of 2,536 complaints resulted in findings. Reporting isn’t futile; over half of investigated complaints are validated.
Federal Reporting Options
When state agencies won’t investigate, OSHA worker-safety complaints provide a federal pathway. Use the OSHA-7 online form with a confidentiality checkbox to keep your name from your employer.
If understaffing constitutes Medicare/Medicaid fraud, DOJ False Claims Act settlements, like the $819,640 Pennsylvania facility case, show whistleblowers can pursue fraud claims with a 15-30% relator recovery.
Whistleblower Protections for CNAs
Federal and state laws protect CNAs who report unsafe conditions, but you must know the critical deadlines and procedures to invoke these protections.
Federal Protections
OSHA Section 11(c) worker protection regulations prohibit retaliation for reporting safety violations – but you have only 30 DAYS from adverse employment action to file a whistleblower complaint. This is the most important procedural deadline for retaliation claims. Missing it typically results in dismissal.
The HIPAA whistleblower exception under 45 CFR § 164.512 permits disclosure to health oversight agencies – facilities cannot retaliate against you for reporting to state survey agencies by claiming HIPAA violations.
State-Specific Protections
California provides additional protections through Labor Code § 6310 (OSHA complaints) and § 1102.5 (reporting violations to government agencies). Oregon statute ORS 441.181 prohibits retaliation for reporting health care facility violations.
What Happens After You Report
Understanding investigation timelines helps set realistic expectations and reduces anxiety about what comes next.
Investigation Process
State survey agencies typically investigate within 30-90 days, depending on the severity of the complaint. California’s 60-day mandate is the fastest; other states take longer. The OIG analysis of nursing home complaint trends shows investigation delays degrade evidence quality – that’s why your contemporaneous personal documentation is so valuable when investigators finally arrive months later.
How to Document Retaliation
CNAs who’ve reported unsafe conditions describe workplace dynamics changing:
- “I was supposed to report to the same nurse again this morning, but she was put on the other section…she came in and was being all buddy-buddy buddy trying to make small talk…”
- (1056 upvotes – Reddit user)
Document any changes in your work environment post-report: sudden schedule changes, isolation from coworkers, increased scrutiny of your work, verbal warnings for minor issues, or assignment to the most difficult residents. This creates the pattern of retaliation that investigators need to see.
Legal Case Studies: When Documentation Saved (or Failed) CNAs
Real enforcement outcomes prove documentation isn’t theoretical – it’s legally actionable protection.
California: Facilities Fined for Falsified Records
California Elder Abuse Advocates’ 2011 investigation found Santa Monica facility paid $2,500 for 28 phantom therapy sessions documented on days staff weren’t present. Investigators cross-checked documentation with payroll records. The Sylmar facility paid $800 for falsified medication records showing drugs not in the facility’s inventory.
This isn’t a policy violation – it’s billing fraud. Your objective, honest documentation protects you from being implicated in fraudulent charting schemes.
Texas: Double-Jeopardy Registry System
Texas operates a dual-registry system creating permanent employment bars: federal Nurse Aide Registry plus state Employee Misconduct Registry. Texas Administrative Code § 550.418 requires facilities check both registries. With 127,418 certified nurse aides in Texas, that’s massive workforce subject to dual-registry risk. Defensive documentation prevents findings that trigger both registries.
Success Stories: Whistleblower Verdicts
Nancy Valla won $27.5 million whistleblower retaliation verdict against Dignity Health. Her meticulous contemporaneous documentation transformed “insubordination” accusations into protected whistleblower activity. The Iowa Supreme Court in Wiggins v. Oak Park protected a CNA who refused to falsify records. Defensive documentation created the paper trail proving retaliation, not performance issues.
Red Flags Your Documentation Is Working
You’ll know your documentation strategy is effective when facilities change their behavior. Watch for these indicators:
- Management suddenly provides proper staffing after months of unsafe ratios
- Equipment gets repaired or replaced quickly instead of remaining broken for weeks
- Supervisors start documenting conversations with you in writing (creating their own CYA paper trail)
- You’re asked to sign acknowledgment forms about policies or procedures that have never been mentioned before
- Facility implements new incident reporting systems or documentation requirements
These aren’t coincidences. Your systematic documentation forced facility response. When management realizes you’re creating records they can’t destroy, their risk calculus changes.
Non-Union Alternatives to ADO Forms
You don’t need union membership to create assignment objection records with a legal protective function. Use the Scenario 1 template combined with email confirmation to create business records.
Email documentation strategy: After verbally objecting to unsafe assignment, send an immediate email to supervisor: “Per our conversation at [time], I raised concern about [specific issue]. I accepted the assignment as directed, but want to document my objection for safety reasons.” This creates a timestamp and a written record they can’t deny receiving.
The NSO guidance on refusing nursing assignments from a professional liability insurance perspective emphasizes that documentation protects against malpractice claims even when you must accept unsafe assignments.
Common Documentation Mistakes That Weaken Your Defense
Batch Charting and Backfilling
NSO analysis of charting-by-exception legal risks explains that phantom charting (documenting care before providing it or after the shift ends) carries higher liability than a negligent omission. California enforcement shows investigators cross-check documentation timestamps with badge swipe data and payroll records.
Document in real-time or as close to contemporaneous as possible. If you must batch chart due to emergencies, note the reason: “Charting delayed due to responding to a fall in Room B, resident required continuous monitoring until RN assessment is complete.”
Documenting in the Wrong Location
Clinician.com risk management guidance warns that documenting staffing shortages in patient medical records can appear as “blame shifting” to juries. Keep two separate systems: clinical documentation in the facility EMR (patient care), and administrative documentation in a personal CYA file at home (staffing, equipment, workplace safety).
Using Facility Language Suggesting Acceptance
Never write “I agreed to” or “I accepted” without documenting your objection. Better phrasing: “Assignment accepted per management direction after expressing safety concerns at [time].” The Washington Department of Health patient abandonment guidance clarifies that you must accept assignments to avoid abandonment charges, but you can simultaneously document your objection.
Your Action Plan: Implementing Defensive Documentation Today
From a veteran CNA to those feeling trapped in hostile facilities:
“I have been a CNA for 13 years…please remember you have soooooo many options…you are damn valuable”
(199 upvotes – Reddit user)
Tonight: Create your personal CYA file folder at home. Label it with a date range. Place in a secure location away from the workplace.
This Week: Implement Scenario 1 template on your next shift if ratios exceed safe standards. Document one shift completely – assignment, staffing, objections, supervisor responses. Experience how quickly documentation becomes a protective habit.
Ongoing: Build systematic documentation practice. Each shift, spend 5 minutes after arriving home updating your personal file. When incidents occur, document the same day while memory is fresh. Review your file monthly to identify patterns facilities can’t deny when presented with months of consistent records.
You’re not powerless. Documentation is control you have when your employer provides none. Every time you create a contemporaneous record management system that can’t be accessed, you reclaim agency in a system designed to sacrifice frontline staff. That paper trail protects your license, validates your experience, and builds the case for safer staffing, whether that’s through internal change, state enforcement, or your transition to a facility that actually protects its staff.
Experienced CNAs: Leverage Your Skills in Higher-Paying Healthcare Roles
Bridge programs designed for working CNAs. Most complete these while maintaining their current job.