If you’re feeling anxious about hand washing for your CNA skills test, you’re experiencing something completely normal and surprisingly common. Despite seeming like a basic skill, hand washing causes genuine worry because of strict 20-second timing requirements, complete coverage expectations, and the pressure of performing perfectly under evaluator observation.
Students often find that achieving proper hand coverage is more challenging than expected. Even immediately after training, only 72% of healthcare workers achieve satisfactory coverage of all hand surfaces.
Many CNAs express this exact sentiment: “Also, my skills were the easiest, but I was so nervous.” This anxiety makes complete sense when you understand that hand washing appears on every CNA skills test, and a single mistake can result in automatic failure.
What CNAs Need to Know About Hand Washing Requirements
Hand washing isn’t just tested – it’s the foundation of every skill you’ll perform. All three major testing providers (NNAAP, Prometric, and Headmaster) require a minimum 20-second scrubbing time with complete coverage of hands, wrists, and fingers.
Students consistently discover that testing differs significantly from practice: “We actually had to do everything and use real supplies. The only thing we were allowed to verbalize was handwashing, and only after we had demonstrated the skill for real.”
Real Supplies vs. Practice Simulations
This reality means you can’t simply go through the motions. Testing providers maintain strict protocols because hand hygiene directly impacts patient safety, making this skill non-negotiable for certification.
Working CNAs often mention that “they’re going to check up and make sure you still know proper procedures for things like hand washing” – emphasizing that this foundation skill remains critical throughout your career.
The universal 20-second requirement exists across all providers because shorter scrubbing times fail to remove pathogens effectively. Program directors notice that students who understand the reasoning behind each step perform more consistently under evaluation pressure.
Master This Skill With Expert Video Guides
Join 6,000,000+ students who passed with Mometrix’s proven study system
Get Instant Access →Step-by-Step Hand Washing Technique for CNA Testing
Experience shows that students who practice this specific sequence perform better under pressure than those who use general handwashing habits. Each step includes the testing insight that makes the difference between passing and failing.
The Complete 12-Step Testing Sequence
- Turn on the water and adjust the temperature
– Use comfortably warm water – hot water makes you rush through scrubbing
– Testing insight: Evaluators check that you adjust the temperature before wetting your hands - Wet hands completely with fingertips pointing downward
– Keep your hands lower than your elbows throughout the process
– Testing insight: This position prevents recontamination and is specifically observed - Apply a palm-sized amount of soap
– Too little soap reduces lather effectiveness for the full 20 seconds
– Testing insight: Evaluators notice insufficient soap, leading to inadequate coverage - Begin systematic scrubbing for a minimum of 20 seconds
– Count slowly: “one-thousand-one, one-thousand-two” to maintain timing
– Testing insight: This is where 28% of students fail – practice the count until automatic - Scrub palms together with fingers interlaced
– Covers the commonly missed areas between fingers
– Testing insight: Between-finger areas are checked on evaluation forms - Scrub the backs of your hands with the opposite palm
– The dorsal hand surface is missed by 24% of healthcare workers
– Testing insight: Evaluators specifically watch for thorough back-of-hand coverage - Clean under fingernails against the opposite palm
– Fingertip areas are critical for patient contact scenarios
– Testing insight: Nail cleaning is a separate checkpoint on most evaluation forms - Scrub wrists in circular motions
– Often forgotten but specifically evaluated by all testing providers
– Testing insight: Wrist coverage separates thorough students from rushed ones - Rinse thoroughly with fingertips still pointing downward
– Prevents recontamination from water running back up arms
– Testing insight: Hand position during rinsing is observed – maintain downward angle - Dry your hands completely with a clean paper towel
– Incomplete drying can harbor remaining pathogens.
– Testing insight: Evaluators check that you dry between fingers, not just palms - Use a paper towel to turn off the faucet
– Critical step that prevents recontamination of clean hands
– Testing insight: This is an automatic failure point if done incorrectly - Dispose of a paper towel without touching the sink
– Final contamination prevention step
– Testing insight: Any contact with sink surfaces after cleaning results in failure
Students consistently struggle with maintaining the 20-second timing when nervous, which is why understanding the rhythm beforehand makes such a difference. Practice counting while scrubbing until the timing becomes automatic rather than conscious.
Practice With 600+ CNA Exam Questions
See exactly how this skill appears on the real test
Interactive Hand Washing Practice Checklist:
Perfect your technique before test day with this comprehensive checklist based on official evaluator scoring criteria. The interactive format includes a 20-second timer to help you practice proper timing while ensuring complete coverage of all hand surfaces.
Download the complete PDF checklist to practice offline and bring confidence to your skills test. This tool mirrors evaluators’ exact steps to score your performance across all testing providers.
Managing Hand Washing Performance Under Observation
The psychological aspect of hand washing under observation affects everyone differently, but understanding why it happens helps you prepare. Research shows that observation pressure creates three times the normal behavioral changes in healthcare workers.
Why Observation Pressure Affects Performance
Many CNAs discover that the real challenge isn’t handwashing itself—it’s performing it perfectly while someone watches and takes notes. Students frequently report, “Getting nervous when evaluators watch closely affects performance even when students know the procedures well.”
This concern appears throughout the profession: “I had a lot of anxiety and questions I couldn’t really find answers for.” The response is completely normal because your brain recognizes the high stakes of the testing situation.
Practical Strategies for Observation Management
Timing Techniques When Nervous:
- Practice with a visible timer until 20 seconds feels natural
- Use the “one-thousand” counting method even during practice
- Remember that going slightly over 20 seconds is better than rushing
Maintaining Focus Under Scrutiny:
- Breathe normally – holding your breath increases tension
- Focus on your hands rather than the evaluator
- Treat the evaluator as a learning partner, not a judge
Mental Preparation Strategies:
- Visualize successful handwashing the night before testing
- Practice the sequence until it becomes muscle memory
- Remember that evaluators want you to succeed
Testing providers notice that confident students often perform better, not because their technique is superior, but because they maintain consistent timing and thoroughness despite observation pressure.
Common Hand Washing Mistakes That Cause Test Failures
Understanding specific failure patterns helps you avoid the mistakes that trip up other students. Program directors consistently see the same errors across different CNA programs.
Critical Recontamination Errors
Touching sink surfaces after washing (automatic failure):
- Affects approximately 15% of test-takers
- Prevention: Use a paper towel for all contact with the faucet and sink area
- Remember: Once hands are clean, they stay clean until the skill is complete
Improper faucet shutdown technique:
- The second most common critical error
- Prevention: Keep a paper towel in hand specifically for faucet control
- Never touch faucet handles with bare skin after washing
Coverage Failures by Area
Missed dorsal hand areas (24% of students):
- Often occurs when rushing through back-of-hand scrubbing
- Prevention: Spend equal time on both palm and back surfaces
- Visual check: Ensure you feel soap lather on all back-of-hand surfaces
Inadequate palm coverage (18% of students):
- Usually results from insufficient interlaced finger scrubbing
- Prevention: Interlace fingers completely and scrub palm-to-palm
- Remember: Palm surfaces must be visibly soapy throughout scrubbing
Neglected fingertip areas (3.5% of students):
- Small percentage, but critical for patient contact
- Prevention: Dedicate specific time to nail and fingertip scrubbing
- Technique: Use the opposite palm as a scrubbing surface for fingertips
Timing and Rhythm Issues
Students often underestimate how cognitive load affects their usual handwashing rhythm. When concentrating on being observed, many people unconsciously speed up their movements.
Rushing through the 20-second requirement:
- Most common timing error under pressure
- Prevention: Count out loud (if allowed) or use deliberate, slow movements
- Recovery: If you realize you’ve rushed, continue scrubbing to reach full time
Inconsistent scrubbing pressure:
- Occurs when nervous tension affects hand movements
- Prevention: Practice maintaining steady, moderate pressure
- Focus on thorough coverage rather than aggressive scrubbing
Testing Provider Requirements: NNAAP vs Prometric vs Headmaster
Each testing provider uses the same core requirements but differs in evaluation approach and specific protocols. Understanding these differences helps you prepare for your specific testing situation.
NNAAP (Credentia/Pearson VUE) Protocol
Timing Requirements:
- Minimum 20 seconds of lathering with friction
- Hands must remain below elbows with fingertips downward
Critical Failure Points:
- Insufficient scrub time (automatic failure)
- Any recontamination through sink or faucet contact
- Missing any critical element step marked in bold on the checklist
Evaluation Approach:
- Evaluators use a standardized checklist with critical steps clearly marked
- After the initial handwashing demonstration, subsequent hand hygiene can be verbalized
- No coaching or prompting provided during testing
Prometric Standards
Six-Checkpoint System:
- Wetting hands and applying soap before cleaning
- Using friction on all hand surfaces, including wrists
- Scrubbing for a minimum of 20 seconds
- Rinse all soap from hands and wrists
- Drying with a clean paper towel
- Avoiding recontamination throughout the process
Evaluation Specifics:
- All six checkpoints must be satisfied for passing
- Some states use dual evaluator observation
- Hand hygiene between skills is evaluated under “Indirect Care.“
Headmaster (D&S Diversified) Approach
Scenario-Based Integration:
- Hand washing embedded within care scenarios
- Some scenarios specifically require a “with Hand Washing” demonstration
- Routine hand hygiene is performed with sanitizer during most skills
Key Differences:
- Uses scenario format rather than standalone skill testing
- Combines soap-and-water washing with alcohol-based sanitizer use
- RN Test Observer uses a detailed checklist for full washing scenarios
COVID-Era Adaptations:
- Increased use of hand sanitizer for routine hygiene moments
- At least one scenario requires a complete soap-and-water demonstration
- Safety protocols are maintained while preserving core technique requirements
Universal Requirements Across All Providers
Despite approach differences, all providers maintain identical core standards:
- 20-second minimum scrubbing time
- Complete hand, wrist, and finger coverage
- Fingertips pointing downward during rinsing
- No recontamination after cleaning
- Proper paper towel use for faucet control
Program directors tell us that confidence comes from knowing exactly what evaluators look for, not just hoping your technique is good enough.
| Testing Provider | Key Requirement | Critical Failure Points | Unique Feature |
|---|---|---|---|
| NNAAP | 20-second minimum friction | Re-contamination, insufficient time | Verbalization after initial demo |
| Prometric | 6-checkpoint system | Any checkpoint failure | Dual evaluator observation |
| Headmaster | Scenario-based integration | Same core standards | Sanitizer + soap combination |
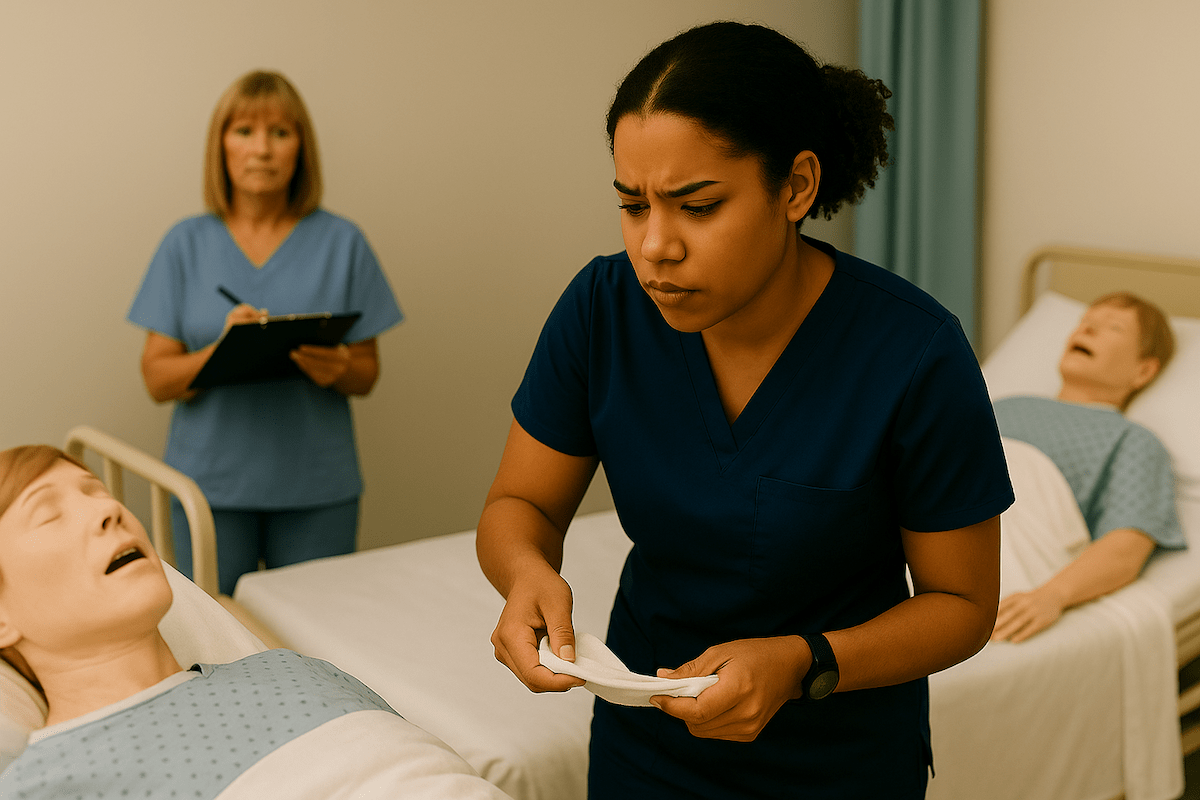
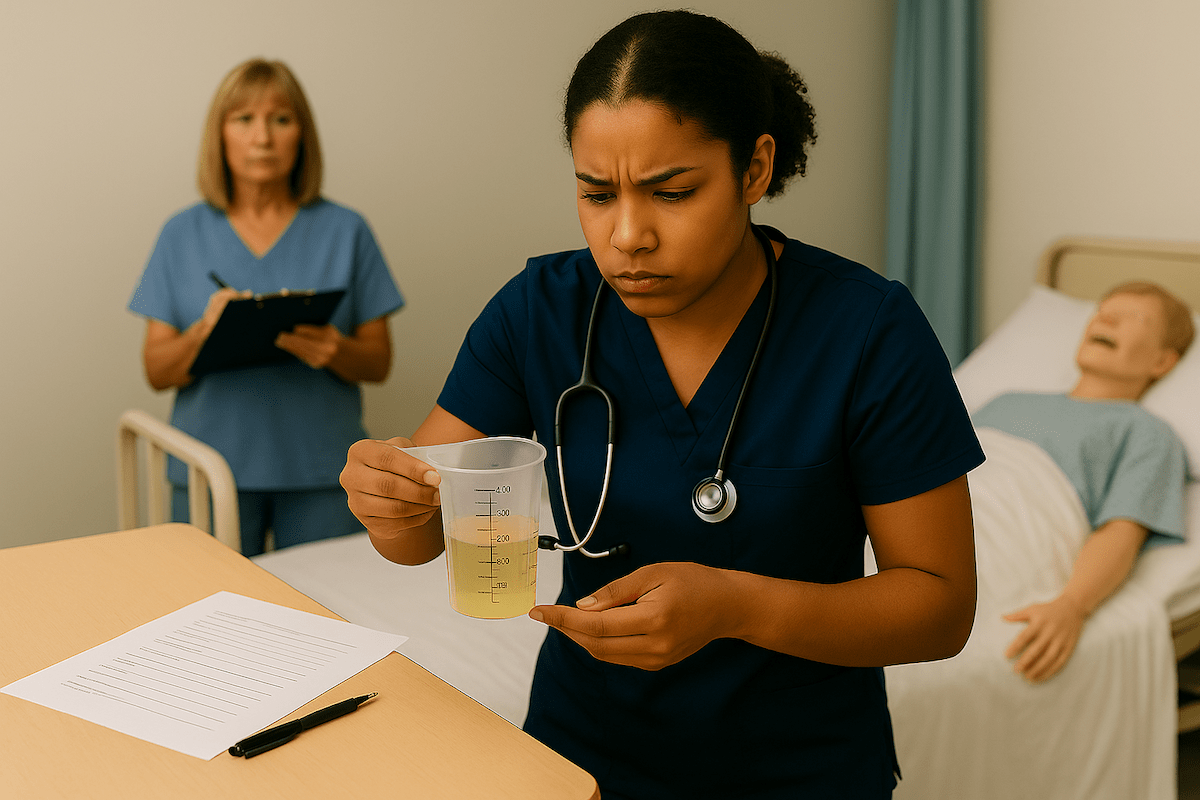
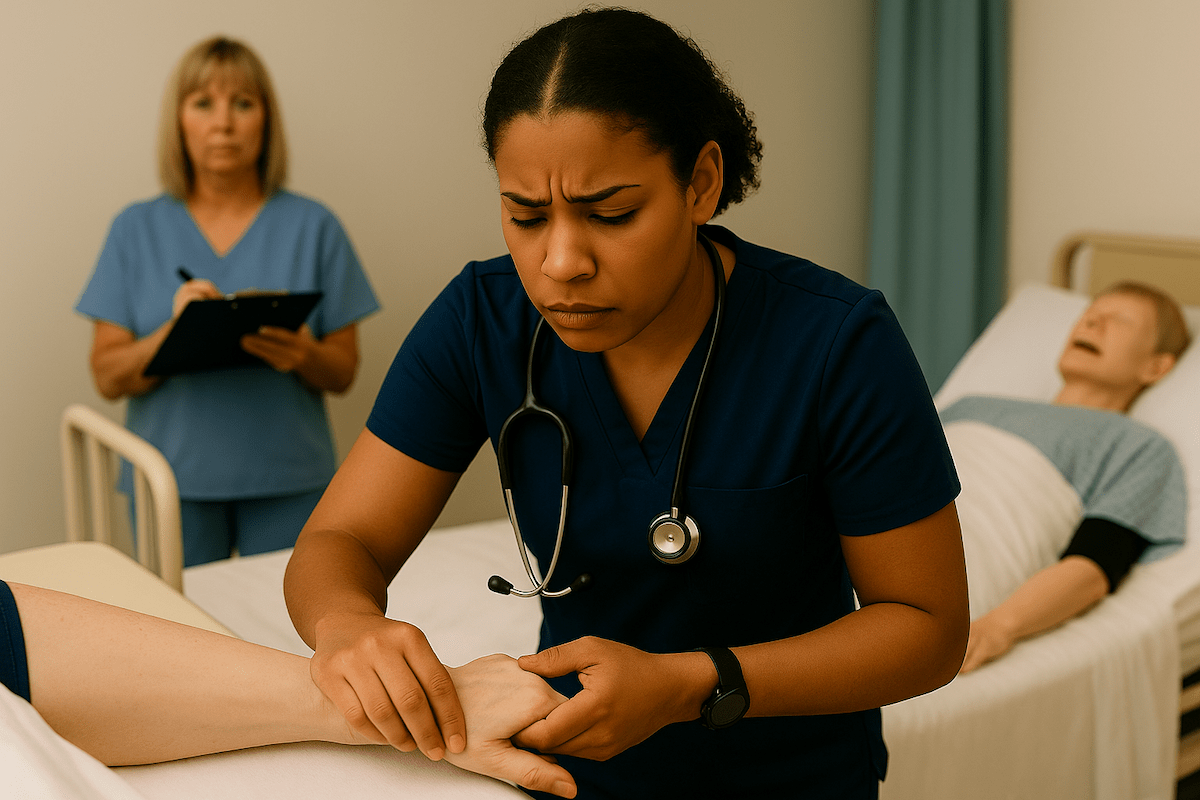
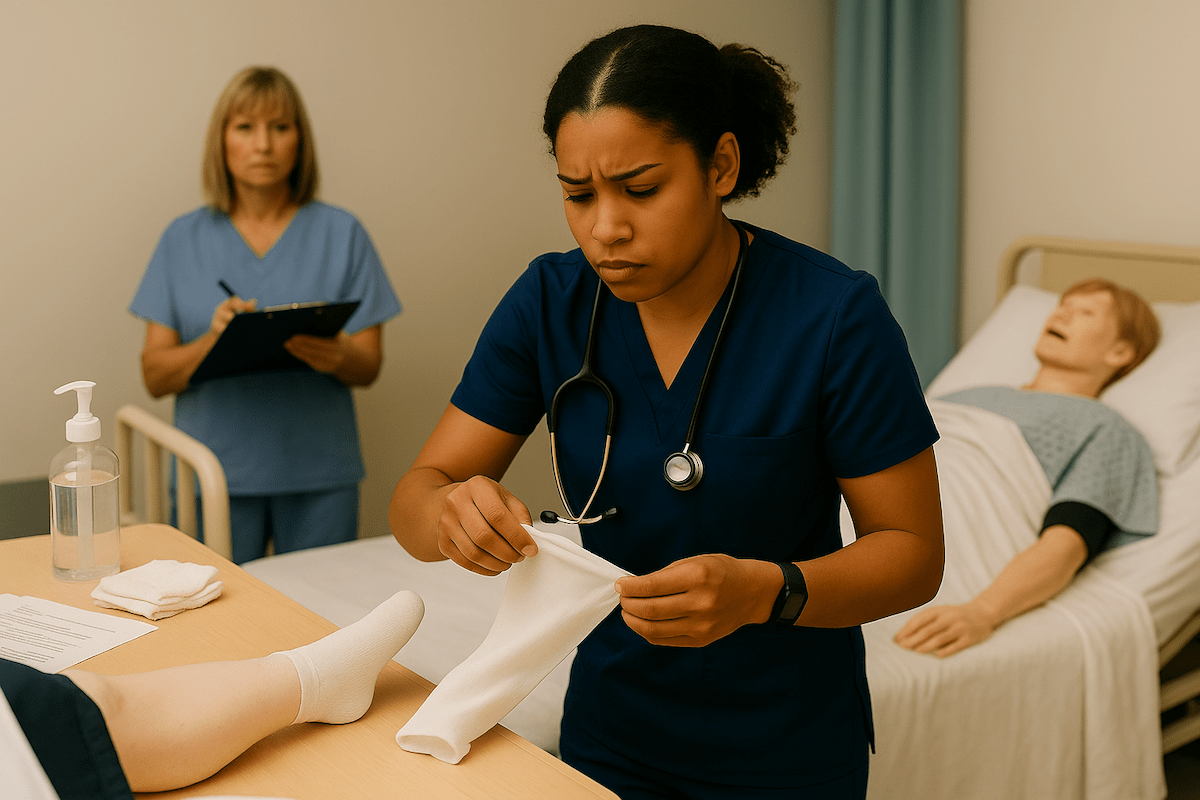
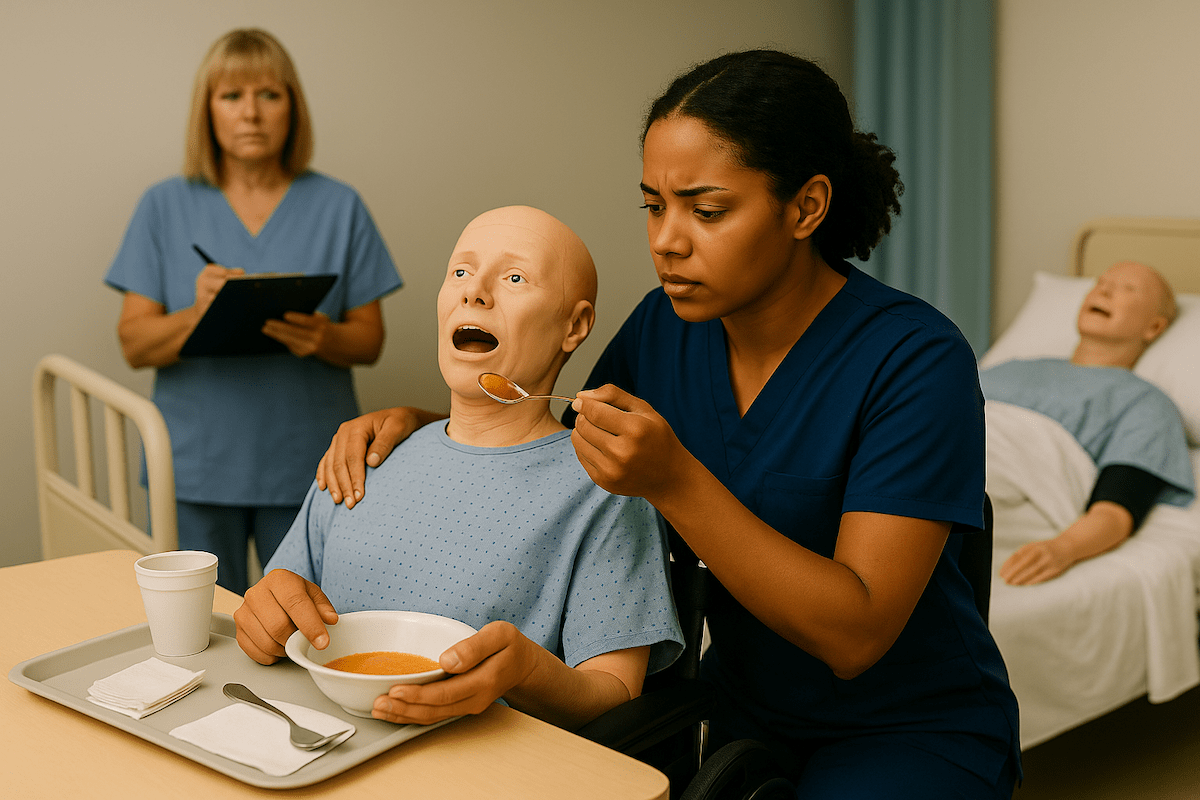
Hand Washing Video Demonstrations
These demonstrations reinforce the written instructions above by demonstrating proper action techniques. Our research with CNA students shows that combining written guidance with visual learning significantly improves technique retention and test-day confidence.
These videos demonstrate the exact hand positioning, timing, and coverage patterns evaluators look for across all testing providers. Watch for the systematic approach to coverage and contamination prevention that separates passing performances from failures.
Hand Washing FAQ for CNA Students
All testing providers require a minimum of 20 seconds of active scrubbing with soap and water. This timing aligns with CDC guidelines for effective pathogen removal.
Use a clean paper towel to operate faucet handles, preventing recontamination of freshly washed hands. Never touch faucets with bare, clean hands.
Touching the sink basin with clean hands is considered critical recontamination and typically results in automatic failure of the hand hygiene skill.
No. All providers require demonstration of proper soap and water technique. Sanitizer may be used for routine moments in some formats, but it cannot be substituted for the scored hand washing skill.
After the initial hand washing demonstration, most providers allow verbalization (“I would wash my hands now”) rather than physical washing between skills.
Evaluators are trained to observe timing as part of standardized scoring. Insufficient scrubbing time typically results in skill failure.
Ready to Ace Your CNA Exam?
Get everything you need: video guides, practice tests, and detailed study plans