If you’re feeling anxious about performing bed bath care under RN observation, that concern makes complete sense – this skill requires both technical precision and compassionate patient interaction during evaluation. The encouraging reality is that understanding exactly what evaluators look for can transform your confidence from anxiety to competence. Students who master provider-specific requirements consistently report feeling more prepared and less stressed during their skills testing.
What CNAs Need to Know About Bed Bath Requirements
Why CNAs Prefer Bed Baths Over Showers
Many CNAs discover that bed baths often provide more thorough patient care than shower alternatives, despite initial assumptions. One CNA community member shared: “I absolutely hate giving showers. It’s hot, steamy, my scrubs get wet, and it’s very time-consuming… I would really rather do a complete bed bath.”
This preference reflects practical advantages that extend beyond personal comfort to genuine patient care quality.
Universal Testing Requirement Across All Providers
Bed bath skills appear on every CNA evaluation across all major testing providers – NNAAP, Prometric, and Headmaster. Each provider emphasizes patient dignity and infection control, but their specific requirements vary significantly.
Understanding these distinctions prevents automatic failures that catch unprepared students off guard.
Clinical Evidence Supporting Proper Technique
Clinical research demonstrates why healthcare facilities prioritize proper bathing techniques. ICU daily CHG bathing reduces bloodstream infections by 44%, and non-ICU device patients experience 32% fewer BSIs with daily CHG protocols.
These statistics reflect the serious responsibility CNAs carry when providing patient hygiene care.
Frequency Standards by Healthcare Setting
Healthcare settings establish different frequency standards based on patient acuity and evidence-based protocols. ICU patients typically receive daily full-body baths with CHG, while long-term care residents follow individualized care plans averaging 2-3 times weekly.
Understanding these variations prepares you for real-world practice beyond testing requirements.
INFECTION PREVENTION IMPACT: Daily CHG bathing reduces ICU bloodstream infections by 44% and non-ICU device-related infections by 32%, demonstrating why proper technique matters beyond testing success.
Master This Skill With Expert Video Guides
Join 6,000,000+ students who passed with Mometrix’s proven study system
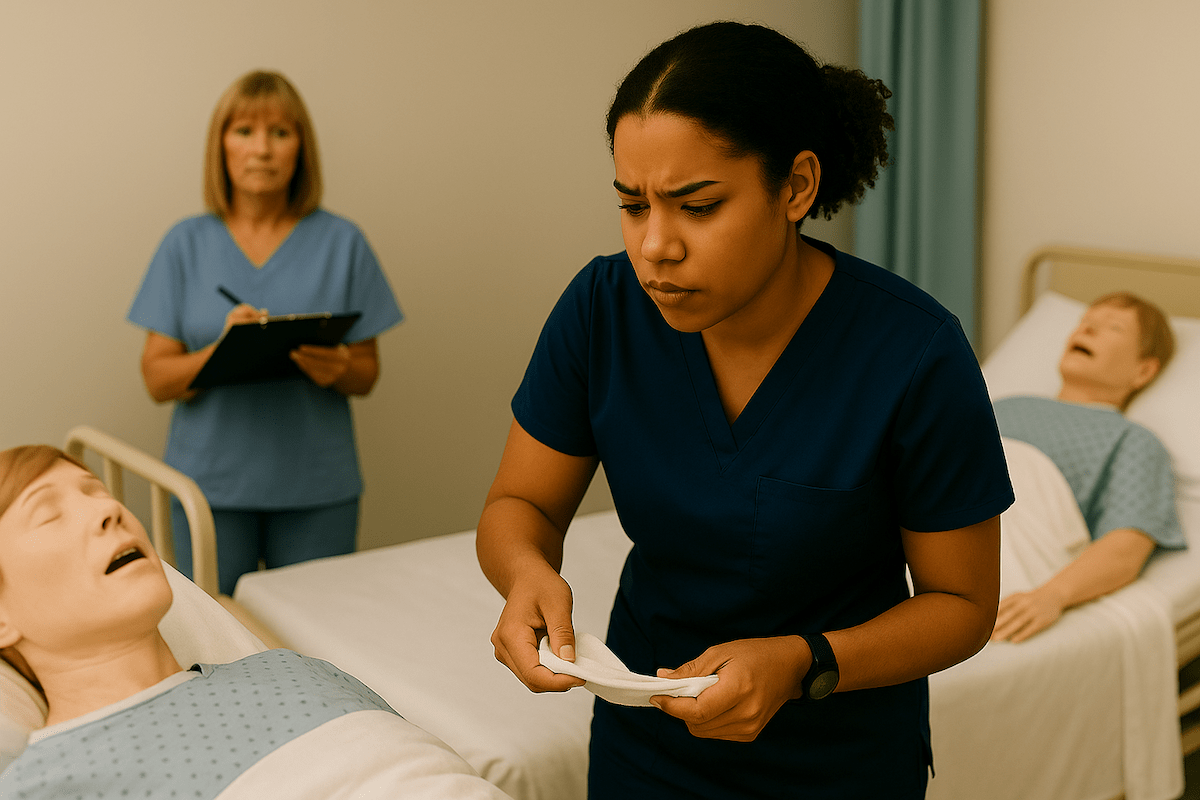
Get Instant Access →Step-by-Step Partial Bed Bath Technique for CNA Testing
Testing providers evaluate bed bath skills through specific checklists, but the foundational approach remains consistent across settings. Proper preparation prevents the most common failure points while ensuring patient comfort throughout the procedure.
Provider-Specific Requirements Comparison
| Provider | Scope | Critical Requirements | Automatic Failure Points |
| NNAAP | Face and one arm only | Water temp + client verification, inner→outer eye care | Missing any Critical Element Step |
| Prometric | Face, arm, neck, chest, abdomen + back rub | Soap-free face wash, warm lotion | Poor indirect care behaviors |
| Headmaster | Face and one arm | Towel under arm, contamination control | Hand hygiene, safety violations |
Complete 15-Step Procedure Guide
- Knock and identify yourself by name to the patient
Why this matters: Evaluators score communication and professional courtesy from the first interaction. Missing this step signals poor bedside manner.
- Explain the complete procedure before beginning
Testing insight: Prometric heavily weights indirect care behaviors. Students who skip explanations lose significant points even with perfect technique.
- Wash your hands thoroughly and put on gloves
Critical for testing: Hand hygiene before patient contact prevents automatic failure across all providers. Evaluators watch for this immediately.
- Provide privacy by closing the curtain or door completely
Why this matters: Privacy violations cause automatic failure. Partial closure isn’t sufficient – evaluators need complete visual barriers.
- Adjust the bed to a comfortable working height and lock all wheels
Safety requirement: Unlocked wheels create safety hazards that result in immediate point deductions. Working height prevents your back from straining during extended procedures.
- Place a bath blanket over the patient and ask them to hold it
Dignity protection: This step maintains patient modesty during gown removal. Students who expose patients inappropriately fail this skill immediately.
- Remove the patient’s gown while keeping them covered with a blanket
Testing technique: Keep chest and lower body covered throughout. Remove arms from sleeves carefully without exposing sensitive areas.
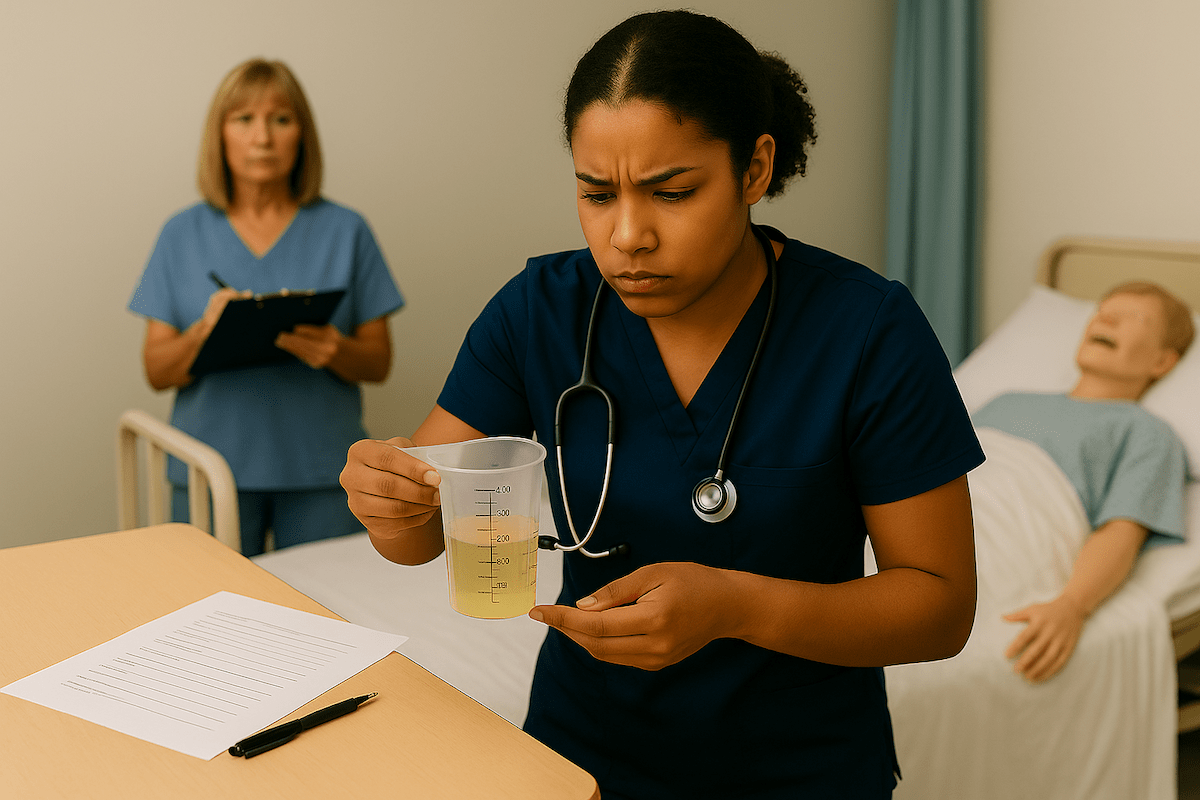
- Fill the basin with warm water and test the temperature with a thermometer
A temperature range of 98-105°F is safe. Water that’s too hot causes burns; water that is too cool creates patient discomfort and evaluation point loss.
- Ask the patient to verify the water temperature comfort
Dual verification required: All providers require both thermometer testing AND patient confirmation. Missing either step causes failure.
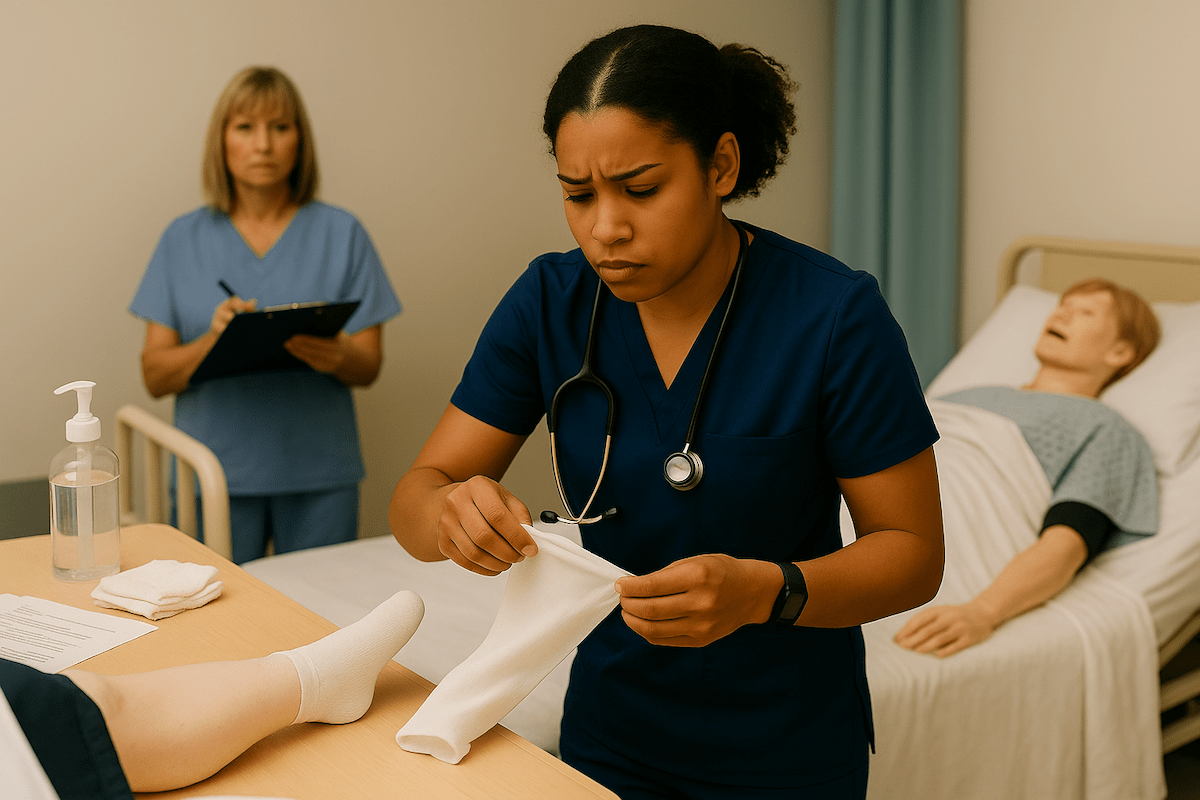
- Place a towel under the body part being washed (Required for Headmaster)
Contamination control: This demonstrates infection prevention awareness. Other providers appreciate this technique even when it is not mandatory.
- Wash the patient’s eyes from the inner corner to the outer corner
Critical technique: Use a different washcloth area for each eye and each stroke. Wrong direction or cloth reuse causes automatic failure.
- Clean face without soap, then wash ears and neck
Universal requirement: Soap-free face washing prevents eye irritation. Using soap on the face results in immediate failure across all providers.
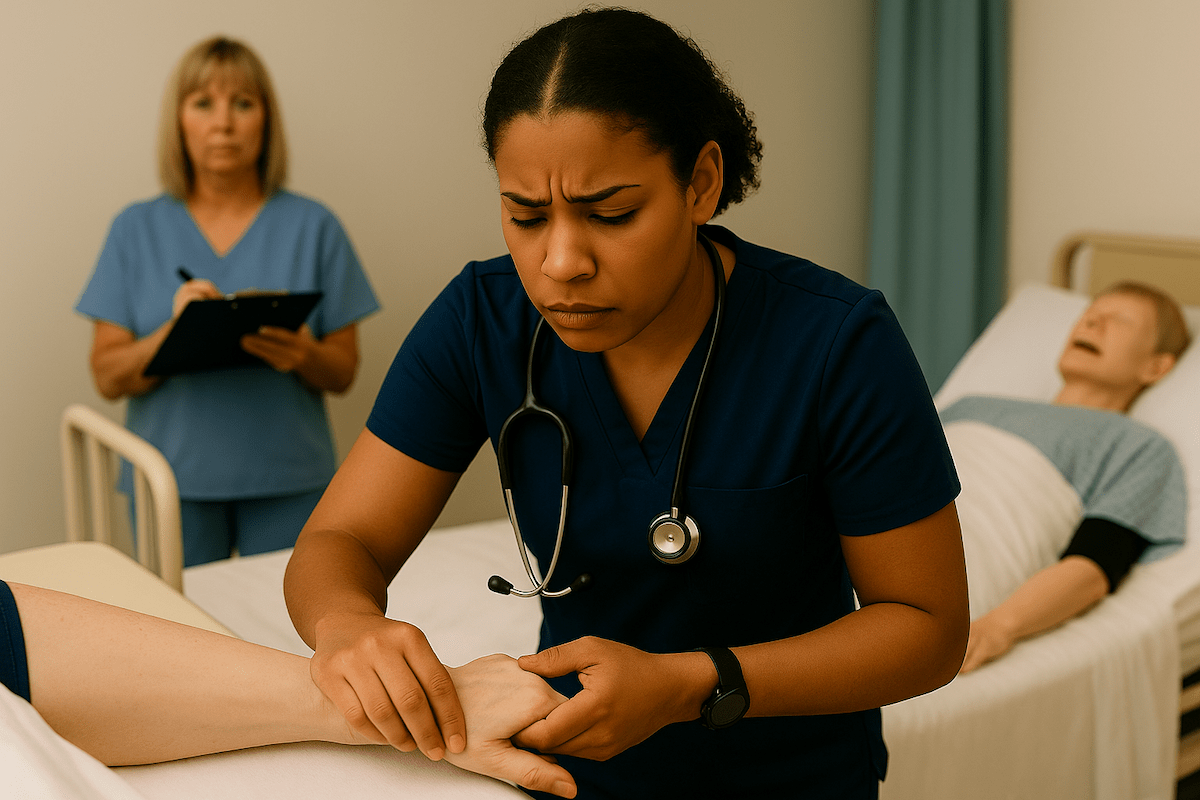
- Wash one arm from shoulder to wrist using long, smooth strokes
Circulation benefit: Long strokes promote blood flow while ensuring thorough cleaning. Short, choppy motions appear unprofessional to evaluators.
- Clean the patient’s hands, including under fingernails
Infection prevention: Nail cleaning prevents bacterial accumulation. Use an orangewood stick or nail brush when provided by the testing facility.
- Complete safety procedures: clean gown, bed lowered, call light within reach, hand hygiene
Testing success: Students who rush through finish procedures often fail despite perfect technique. Each safety step carries equal evaluation weight.
Back Rub Integration (Prometric Requirement)
Prometric evaluations require back rub integration with specific technique standards. This addition distinguishes Prometric from other providers and requires additional preparation.
Lotion Warming Technique:
- Warm lotion between palms before application
- Cold lotion creates patient discomfort and evaluation point loss
- Apply with long, gliding motions from neck to lower back
Massage Pressure Guidelines:
- Use firm but gentle pressure throughout
- Circular motions at the shoulder blades and lower back
- Maintain communication about patient comfort preferences
Students often underestimate back rub timing requirements. Plan an additional 5-7 minutes for proper technique execution that satisfies Prometric evaluation standards.
Practice With 600+ CNA Exam Questions
See exactly how this skill appears on the real test
Interactive Bed Bath Skills Checklist
Our interactive bed bath checklist transforms the comprehensive technique steps above into a hands-on practice experience that mirrors real testing conditions. This digital tool allows you to work through each critical element systematically and identify any gaps in your preparation before they become testing failures.
The downloadable PDF version provides the same comprehensive checklist in a portable format perfect for clinical practice sessions and last-minute review. Print multiple copies to practice with study partners or keep in your clinical bag for quick reference during training rotations.
Managing Performance Anxiety During Bed Bath Evaluation
Testing anxiety around intimate patient care affects most CNA students, regardless of age or background. Understanding evaluator expectations transforms nervous energy into focused preparation.
RN Evaluator Observation Reality
All three major providers use RN evaluators who understand the emotional challenge of observed intimate care. These professionals evaluate technical competence while recognizing the learning process inherent in certification testing.
What Evaluators Actually Watch:
- Patient dignity maintenance throughout the procedure
- Infection control consistency at each step
- Communication quality during vulnerable patient interactions
- Safety awareness, including bed positioning and hand hygiene
What Evaluators Don’t Expect:
- Perfect speed or efficiency during testing
- Conversational ease with unfamiliar patients
- Advanced clinical judgment beyond basic competency
Anxiety Management Strategies
Before Evaluation Day: Practice explaining each step aloud until narration feels natural. Many students report that verbal processing reduces performance pressure during actual testing.
During Patient Interaction: Focus on patient comfort rather than evaluator presence. Students who prioritize patient experience consistently score higher on indirect care behaviors.
Breathing Technique for Nervous Moments: Use controlled breathing between procedure steps. This technique maintains steadiness without appearing unprofessional to evaluators.
A CNA shared in community discussions: “She started crying and said to me that she was thankful I helped her. And that they rarely come by her room to help her.” This emotional impact reminds students why bed bath competency matters beyond testing success.
Common Bed Bath Mistakes That Cause CNA Test Failures
Testing failure patterns repeat consistently across providers, making prevention strategies highly effective for prepared students.
The 8 Most Common Failure Points
1. Privacy and Dignity Violations
- Leaving curtains open or doors unsealed
- Exposing the chest or genitals during gown removal
- Prevention: Check privacy before starting, maintain coverage throughout
2. Water Temperature Verification Errors
- Skipping thermometer check completely
- Testing temperature, but not confirming with the patient
- Prevention: Always do both – test AND ask patient to verify comfort
3. Eye Care Technique Mistakes
- Using soap on the face or eyes
- Wrong direction (outer to inner instead of inner to outer)
- Same washcloth area for both eyes
- Prevention: Practice “inner to outer, different area each stroke” until automatic
4. Critical Element Violations (NNAAP)
- Missing any step marked in bold on the evaluation sheet
- Prevention: Memorize which steps cause automatic failure for your provider
5. Contamination Control Failures
- No towel placement under body parts (Headmaster requirement)
- Touching used linens to clean a uniform
- Wet linens left on the patient
- Prevention: Plan linen management before starting the procedure
6. Incomplete Safety Procedures
- Forgetting to lower the bed after completion
- Call light placement out of the patient’s reach
- Missing hand hygiene after glove removal
- Prevention: Create a mental checklist of finish requirements
7. Poor Indirect Care Behaviors (Prometric Focus)
- Minimal communication during the procedure
- Ignoring patient comfort or preferences
- Rushing through steps without explanation
- Prevention: Practice explaining actions and checking comfort regularly
8. Provider-Specific Requirement Misses
- Prometric: Forgetting soap-free face wash or lotion, warming
- Headmaster: Missing towel barriers or contamination controls
- NNAAP: Violating any Critical Element Step
- Prevention: Know your specific provider’s unique requirements
Failure Prevention Checklist
Before testing, verify you can demonstrate:
- Privacy establishment and maintenance
- Dual water temperature verification
- Soap-free face washing technique
- Inner→outer eye with a clean cloth areas
- Provider-specific requirements (towel barriers, lotion warming, etc.)
- Complete safety finish (bed low, call light, hand hygiene)
One healthcare worker noted: “After the shower, he was STILL dirty, so I did the rest as a bed bath, doing ALL of this in FULL PPE” – this experience highlights why thorough technique matters for both testing and patient care quality.
Complete vs. Partial vs. Modified Bed Bath Differences
Understanding scope variations helps students prepare for testing while building knowledge for professional practice across healthcare settings.
Scope Definitions by Provider
Modified Bed Bath (NNAAP):
- Face and one arm, and underarm only
- 15-20 minute time allocation
- Focus on technique precision over speed
Partial Bed Bath (Prometric):
- Face, arms, neck, chest, abdomen
- Includes a mandatory back rub with warm lotion
- 25-30 minute time allocation
Complete Bed Bath (All Providers for Advanced Skills):
- Full body, including perineal care
- 45-60 minute procedure
- Requires additional infection control protocols
Evidence-Based Frequency by Healthcare Setting
| Setting | Typical Frequency | Method Preference | Clinical Rationale |
| ICU | Daily full-body bath | CHG cloths/solution | 44% reduction in bloodstream infections |
| Med-Surg | Daily hygiePre-packaged clothes | hess preferred | Avoids basin contamination (66-98% harbor pathogens) |
| Long-Term Care | 2-3x weekly + PRN | Resident preference-based | No federal minimum, individualized care plans |
| Home Health | Plan of care specified | Comfort-focused methods | Must specify frequency, not PRN only |
Method Selection for Safety
Pre-packaged cloths provide safer alternatives to reusable basins in most healthcare settings. Research shows basin contamination rates of 66-98% harbor HAI-linked pathogens, making single-use products preferable when available.
CHG (chlorhexidine gluconate) protocols demonstrate significant infection prevention benefits, particularly for device-bearing patients who experience 32% fewer bloodstream infections with daily CHG bathing.
Students preparing for professional practice benefit from understanding these evidence-based standards that guide real-world care decisions beyond testing requirements.
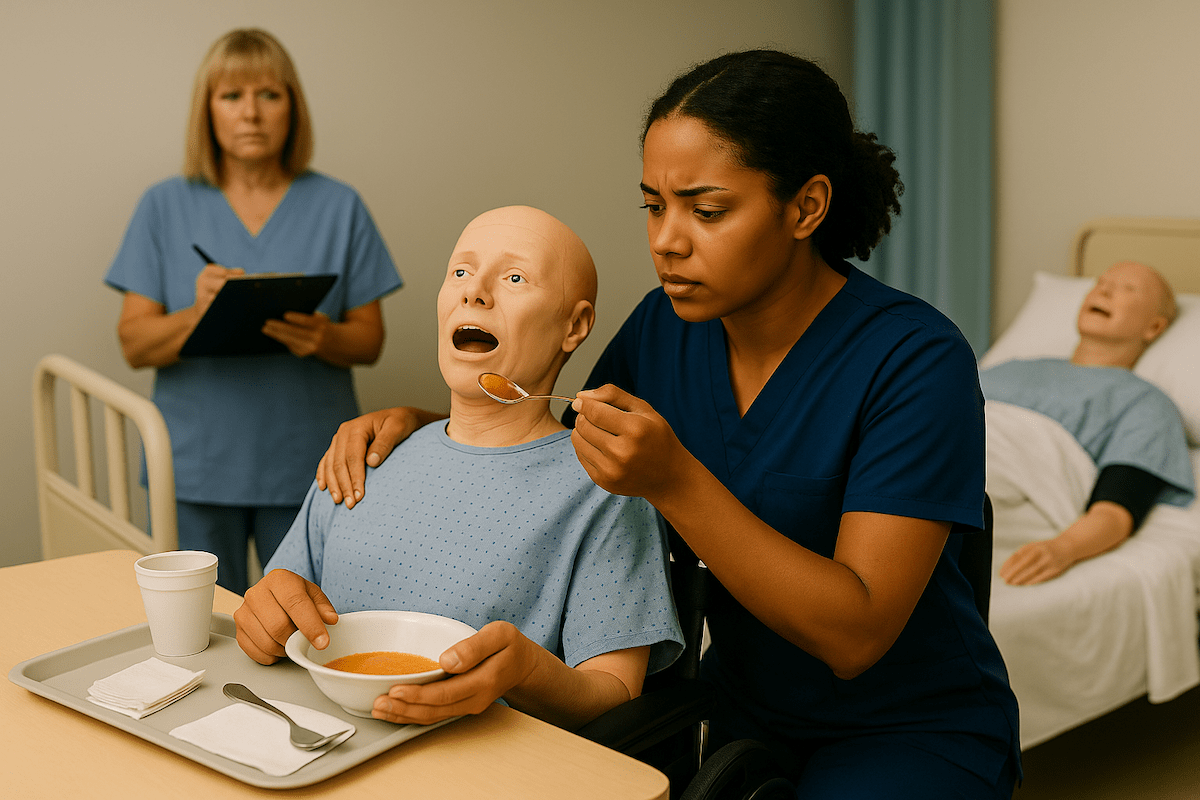
Bed Bath Video Demonstrations
These carefully selected video demonstrations showcase real healthcare professionals executing each critical element with the precision and dignity evaluators expect during testing. The visual examples reinforce the written techniques above while revealing the subtle professional behaviors often determining evaluation success.
Watch for the water temperature verification techniques, precise eye care movements from inner to outer canthus, and contamination control practices that prevent common mistakes. These demonstrations excel at showing the smooth transitions between procedure steps and the natural communication flow that evaluators score as indirect care behaviors.
Bed Bath FAQ for CNA Students
Follow your testing provider’s specific checklist while maintaining patient dignity throughout. Start with face care (soap-free), proceed to arms and upper body, ensure proper water temperature verification, and complete with safety procedures, including bed lowering and call light placement.
A bed bath provides complete hygiene care for patients unable to shower independently. The procedure includes face washing, body cleansing by sections, and maintaining patient privacy while demonstrating infection control principles that prevent healthcare-associated infections.
Begin with privacy and hand hygiene, explain each step to maintain patient comfort, use a soap-free face washing technique, verify water temperature with both thermometer and patient confirmation, wash from clean to dirty areas, and complete with proper linen disposal and safety checks.
NNAAP testing results in automatic skill failure if you miss any Critical Element Step marked in bold. Other providers deduct significant points for major safety violations or dignity breaches. Review your provider’s specific failure criteria before testing.
Frequency depends on the healthcare setting and patient needs. ICU patients typically receive daily baths with CHG for infection prevention. Long-term care follows individualized care plans, averaging 2-3 times weekly. Home health requires a plan of care specification, not PRN only.
Test water with a thermometer for safety range (98-105°F typically), then ask the patient to verify comfort. All testing providers require both verification methods. Change water if it becomes cool, soapy, or dirty during the procedure.
Prometric requires lotion to be warmed between palms before applying a back rub. Other providers don’t specify this requirement, but patient comfort benefits from warm lotion regardless of testing mandates.
Research demonstrates 66-98% of reusable basins harbor HAI-linked pathogens, including enterococci, gram-negatives, and MRSA/VRE. Pre-packaged clothes provide safer alternatives that reduce cross-contamination risks while maintaining hygiene effectiveness.
Ready to Ace Your CNA Exam?
Get everything you need: video guides, practice tests, and detailed study plans